Dry Eye Relief Guide 2025 | Proven Treatment Solutions
TL;DR: Dry eyes affect approximately 16-20 million diagnosed Americans (with up to 150 million experiencing symptoms), but effective relief is achievable through proven strategies, including preservative-free artificial tears, warm compresses, proper eyelid hygiene, omega-3 supplementation, environmental modifications, and professional treatments like IPL therapy at Cannon EyeCare. Early intervention prevents complications and improves quality of life significantly.
Understanding Dry Eyes: More Than Just Irritation
Dry eye syndrome, medically known as keratoconjunctivitis sicca, occurs when your eyes don’t produce enough tears or when tears evaporate too quickly. This increasingly common condition affects millions of Americans, with recent 2025 surveys revealing that up to 47% of Americans experience frequent or occasional dry eye symptoms (approximately 150 million people), while 6.8% have been formally diagnosed (around 16-20 million people).
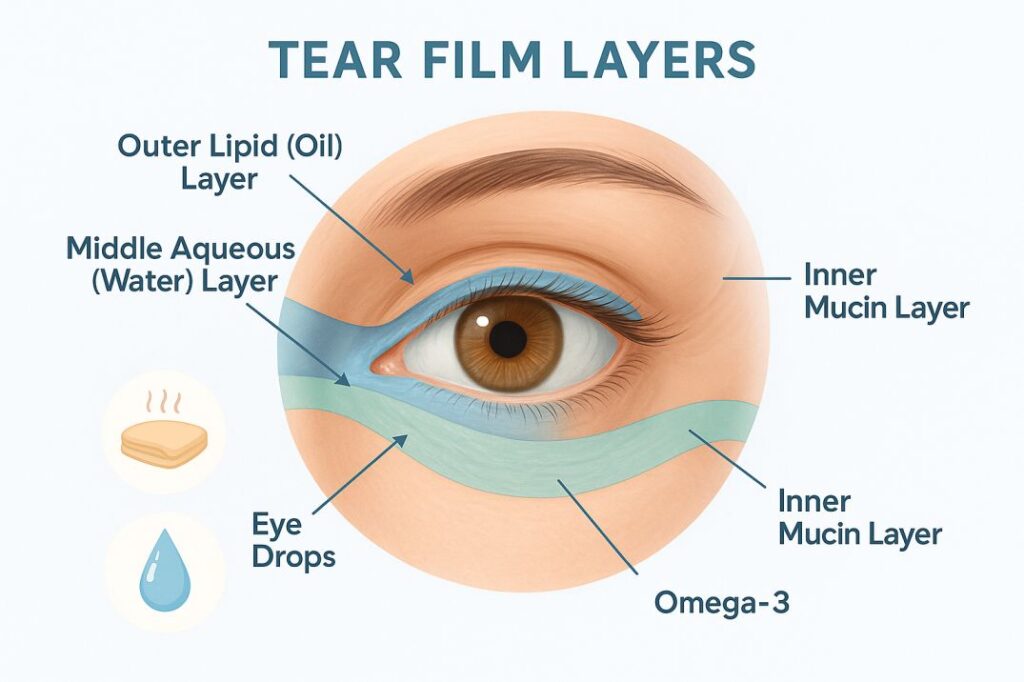
What makes tears so important? Your tear film consists of three essential layers: an oily layer that prevents evaporation, a watery layer that provides nutrients, and a mucus layer that helps tears spread evenly across your eye surface. When any of these layers become disrupted, dry symptoms emerge.
Common Symptoms Include:
- Burning, stinging, or scratchy sensation
- Redness and irritation
- Blurry vision that improves with blinking
- Excessive tearing (a reflexive response to dryness)
- Feeling like something is stuck in your eye
- Light sensitivity
- Eye fatigue, especially during screen time
Evidence-Based Home Remedies for Immediate Dry Eye Relief
1. Preservative-Free Artificial Tears: Your First Line of Defense
Over-the-counter lubricating eye drops remain the most accessible and effective initial treatment for dry eyes. Research consistently shows that preservative-free formulations cause less irritation, especially when used more than four times daily.
What to look for:
- Preservative-free formulations
- Multiple viscosities (thinner drops for daytime, thicker gels for bedtime)
- Brands like Systane Complete and Retaine MGD for enhanced effectiveness
Pro tip: Apply drops before dry eye symptoms worsen, not just when your eyes feel dry.
2. Warm Compresses: Therapeutic Heat for Healthy Glands
Applying warm compresses for at least one minute can help loosen clogged oils in your meibomian glands, which are crucial for preventing tear evaporation. This simple technique addresses one of the most common causes of dry eyes: meibomian gland dysfunction.
Proper technique:
- Use a clean washcloth with warm (not hot) water
- Apply to closed eyelids for 60 seconds to several minutes
- Gently massage eyelid edges to express oils
- Repeat daily, even after dry eye symptoms improve
3. Meticulous Eyelid Hygiene
Proper eyelid cleaning removes debris that can clog tear glands and helps maintain healthy tear film production. This foundational step is often overlooked but critical for long-term eye health.
Daily cleaning routine:
- Mix one part baby shampoo with one part warm water
- Gently massage the solution along the closed eyelid margins
- Pay special attention to the base of eyelashes, where oil glands are located
- Rinse thoroughly with clean water
- Use preservative-free eyelid cleansers for sensitive eyes
4. Strategic Screen Time Management
Digital device use significantly reduces blink rates from a normal 15-20 times per minute to just 3-7 times per minute, dramatically increasing dry eye symptoms. Research shows that incomplete blinking also increases during screen use, further compromising tear film distribution.
The 20-20-20 rule plus:
- Every 20 minutes, look at something 20 feet away for 20 seconds
- Position screens below eye level to reduce the exposed eye surface
- Increase room humidity when using devices
- Take longer breaks every hour
- Consider blue light filtering glasses for extended use
Nutritional and Lifestyle Interventions
Omega-3 Fatty Acids: Anti-Inflammatory Powerhouses
Research suggests omega-3 fatty acids can improve meibomian gland function and reduce dry eye symptoms by decreasing inflammation. While study results are mixed, many patients experience significant improvement.
Best sources:
- Fatty fish: salmon, mackerel, sardines, tuna
- Plant-based options: flaxseed, walnuts, chia seeds
- Quality supplements: 1000-2000mg daily of combined EPA/DHA
Hydration: The Foundation of Tear Production
Adequate hydration supports your body’s natural tear production, with recommendations for 8-10 glasses of water daily. Dehydration directly impacts tear volume and quality.
Hydration strategies:
- Drink water consistently throughout the day
- Include water-rich foods like cucumbers and watermelon
- Limit alcohol and caffeine, which can be dehydrating
- Monitor urine color as a hydration indicator
Environmental Modifications for Lasting Comfort
Combat Dry Air
Using a humidifier adds moisture to indoor air, helping prevent rapid tear evaporation. This intervention is particularly important during winter months when indoor heating systems reduce humidity.
Environmental adjustments:
- Maintain home humidity between 30-50%
- Position humidifiers in frequently used rooms
- Avoid direct air flow from fans, heaters, or air conditioning
- Wear wraparound sunglasses outdoors for wind protection
Air Quality Considerations
Seattle’s unique climate presents both challenges and opportunities for dry eye management. Consider:
- Using air purifiers to reduce allergens
- Avoiding smoke and strong chemical odors
- Taking advantage of Seattle’s naturally humid air when possible
Advanced Treatment Options: When Home Remedies Aren’t Enough
Prescription Medications
When conservative measures prove insufficient, several FDA-approved prescription treatments offer additional relief:
Anti-inflammatory drops:
- Cyclosporine (Restasis): Reduces inflammation and increases tear production
- Lifitegrast (Xiidra): Blocks inflammatory pathways
- Vevye (CyclASol): Recently approved cyclosporine 0.1% solution with improved delivery; typically costs $750-$1,000+ monthly, but patient assistance programs may reduce costs to $59-$0 copay for eligible patients
Newer innovations:
- Miebo (perfluorohexyloctane): FDA-approved in 2023, targets meibomian gland dysfunction specifically by preventing tear evaporation; costs range from $785-$1,300+ monthly, with manufacturer savings programs offering $0 copays for eligible patients
- Reproxalap: Expected FDA approval in 2025, targets aldehydes that amplify inflammation
Professional In-Office Treatments
Intense Pulsed Light (IPL) Therapy: IPL remains a first-choice treatment for dry eyes due to meibomian gland dysfunction, with studies showing a significant reduction in inflammatory markers. This FDA-approved treatment addresses the root cause of evaporative dry eyes.
Other advanced options:
- Punctal plugs to retain natural tears
- LipiFlow thermal pulsation for gland expression
- Radiofrequency treatments for gland function improvement
When to Seek Professional Help
While home remedies provide substantial relief for many people with dry eyes, certain situations require professional evaluation at Cannon EyeCare:
See a Cannon EyeCare specialist if you experience:
- Symptoms persisting longer than a few weeks
- Worsening pain or vision changes
- Symptoms interfering with daily activities
- Unsuccessful relief from over-the-counter treatments
- Signs of infection or severe inflammation
Early evaluation at specialized clinics like Cannon EyeCare helps identify the root cause of dry eyes and prevents complications through timely, targeted therapies.
Seattle-Specific Considerations for Dry Eyes
Climate factors affecting dry eyes in Seattle:
- Seasonal humidity variations
- Indoor heating during the winter months
- Environmental allergens
- Screen-heavy work culture in the tech industry
Local advantages:
- Generally, higher humidity than in many regions
- Access to advanced eye care facilities
- Strong healthcare infrastructure supporting comprehensive treatment
Recent Scientific Evidence Supporting Dry Eyes Treatments
Study 1: IPL Therapy Efficacy for Dry Eyes (2024-2025)
Recent studies demonstrate that IPL therapy significantly improves tear breakup time, meibum quality, and meibomian gland expressibility in patients with MGD-related dry eyes. The treatment shows superior results compared to traditional warm compress therapy alone, with studies showing a significant reduction in inflammatory markers in tears.
Study 2: Omega-3 Supplementation Benefits for Dry Eyes (2024)
Clinical research confirms that omega-3 fatty acid supplementation reduces inflammatory markers in tears and improves dry eye symptom scores when used consistently for 8-12 weeks, though results remain mixed across different studies.
Study 3: Screen Time Impact Assessment on Dry Eyes (2025)
A comprehensive 2025 Bausch + Lomb survey revealed that 75% of dry eye sufferers found the condition “extremely or very bothersome” in daily life, with two-thirds cutting back on activities due to symptoms. Additionally, 88% of patients receiving prescription treatment wished they had started earlier.
Prevention: Building Long-Term Eye Health
Daily habits for healthy eyes:
- Maintain a consistent sleep schedule
- Follow a nutrient-rich diet high in antioxidants
- Practice regular exercise to improve circulation
- Protect eyes from UV radiation
- Schedule annual comprehensive eye exams
Workplace considerations:
- Ensure proper lighting to reduce eye strain
- Position monitors at an appropriate distance and height
- Take regular breaks from concentrated visual tasks
- Use task lighting to supplement overhead lighting
The Bottom Line: Effective Dry Eyes Management is Achievable
Dry eyes relief doesn’t have to be elusive. With the right combination of at-home strategies, lifestyle modifications, and professional care when needed at Cannon EyeCare, most people can achieve significant symptom improvement and prevent complications.
Key takeaways:
- Start with preservative-free artificial tears and proper eyelid hygiene
- Address environmental factors like humidity and screen time
- Consider nutritional support through omega-3 supplementation
- Seek professional evaluation for persistent or worsening symptoms
- Embrace a holistic approach that addresses root causes, not just symptoms
Remember: 88% of patients receiving prescription dry eyes treatment wish they had started treatment earlier. Don’t wait for symptoms to worsen—early intervention leads to better outcomes and improved quality of life.
Expert Care at Cannon EyeCare
At Cannon EyeCare, we understand that dry eyes is more than an inconvenience—it’s a complex condition requiring personalized attention and comprehensive care. Our Seattle-based team combines Midwestern hospitality with cutting-edge diagnostic technology to identify the root causes of your dry eye symptoms.
Why choose Cannon EyeCare for dry eyes treatment?
- Comprehensive medical eye exams focused on dry eye evaluation
- Advanced diagnostic equipment to assess tear quality and gland function
- Personalized treatment plans addressing your specific dry eye needs
- Convenient University Village and Pike Place Market locations
- Insurance acceptance, including Premera, Regence, and other regional plans
Schedule your dry eyes evaluation today to discover which treatment approach will work best for your unique situation. Relief is possible, and Cannon EyeCare is here to help you achieve it.
FAQs
-
Apply a warm compress, blink more often, stay hydrated, and use preservative-free eye drops. Limit screen time and keep your environment humidified for relief