Thermal Therapy for Dry Eye & MGD in Seattle
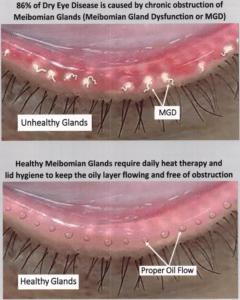
Struggling with dry eyes? 86% of cases link to Meibomian Gland Dysfunction (MGD). Discover how Seattle’s thermal therapies unclog glands and unlock lasting relief—your solution starts here.
 Have you been suffering from Dry eye or MGD? Thermal therapies for dry eye and MGD could be the solution you’re looking for. In this article, you can get all the information you need about Dry Eye and Meibomian Gland Dysfunction (MGD) and how you can treat them with Thermal Therapies for dry eye.
Have you been suffering from Dry eye or MGD? Thermal therapies for dry eye and MGD could be the solution you’re looking for. In this article, you can get all the information you need about Dry Eye and Meibomian Gland Dysfunction (MGD) and how you can treat them with Thermal Therapies for dry eye.
Key Takeaways
-
MGD Is the Primary Culprit: Meibomian Gland Dysfunction is responsible for 86% of dry eye cases, yet remains underdiagnosed and undertreated.
-
Not All Dry Eye Is the Same: Differentiating between evaporative dry eye (from MGD) and aqueous-deficient dry eye is essential for choosing the right treatment.
-
Thermal Therapies Work—But Are Underused: Despite widespread clinical support, only 5% of patients receive thermal gland expression, a proven method to clear blockages and restore tear stability.
-
Blinking Habits Directly Impact Eye Health: Incomplete or weak blinks—especially common during screen time—reduce oil secretion and worsen dryness. Retraining your blink can make a real difference.
-
Gland Atrophy Is Permanent: Once your meibomian glands deteriorate, they can’t regenerate—making early detection and intervention critical.
-
Seattle’s Cannon EyeCare Leads the Way: With advanced imaging, tailored care plans, and expert-led thermal treatments, Dr. Mark Cannon delivers the comprehensive solutions many patients miss elsewhere.
What Is MGD?
Meibomian Gland Dysfunction (MGD) is a condition characterized by the dysfunction or blockage of the meibomian glands, which are located in the eyelids. These glands produce the oily component of the tear film (meibum) that coats the ocular surface, helps lubricate the eyes, and prevents tears from evaporating too quickly.
What Is Dry Eye?
Dry eye, also known as dry eye syndrome, dry eye disease, ocular surface disease, or keratoconjunctivitis sicca, is a common condition that occurs when there is a lack of sufficient moisture or lubrication on the surface of the eyes. It can result from either decreased tear production or increased tear evaporation. Recent studies have shown that about half of Americans will experience dry eye as they age.
Is MGD the Same as Dry Eye? (Understanding the Key Differences)
Meibomian Gland Dysfunction (MGD) and dry eye are often confused due to overlapping symptoms like irritation, burning, and blurry vision. However, they’re distinct conditions with different root causes. Dry eye is categorized into two types: aqueous-deficient dry eye (caused by insufficient tear production) and evaporative dry eye, which is directly linked to MGD.
Evaporative Dry Eye: How MGD Causes Poor Tear Quality
If you have evaporative dry eye, your tears lack the necessary oils to stay stable, causing them to evaporate too quickly. This is why Seattle eye doctors perform a Tear Break-Up Time (TBUT) test, where you hold your eyes open under a blue light for 10 seconds. A TBUT result under 10 seconds signals evaporative dry eye. Key facts:
- 86% of dry eye patients have the evaporative type, often tied to MGD.
- You can have both aqueous-deficient and evaporative dry eye simultaneously.
Advanced MGD Diagnosis in Seattle at Pike Place
At our Pike Place clinic, Dr. Mark Cannon, a trusted dry eye specialist, uses cutting-edge Firefly slit lamp microscope technology to diagnose MGD. This tool captures infrared images of your meibomian glands, allowing precise evaluation of gland health and tear stability. For Seattle residents struggling with dryness, this technology ensures tailored, effective treatment plans.

Evaporative vs. Aqueous Dry Eye: Why the Difference Matters for Treatment
Understanding the difference between evaporative dry eye (linked to MGD) and aqueous-deficient dry eye is critical for effective treatment. Here’s how they compare:
Tear Film Layers: The Foundation of Eye Health
Your tear film has three essential layers:
- Oily Layer (Meibomian Glands): Prevents rapid tear evaporation and ensures a smooth ocular surface.
- Watery Layer (Lacrimal Glands): Makes up the bulk of your tears, providing moisture and protection.
- Mucus Layer (Conjunctiva): Helps spread tears evenly across the eye.
How MGD Disrupts the Oily Layer
In Meibomian Gland Dysfunction (MGD), glands become clogged or produce thick, poor-quality oils (similar to butter or Crisco). This leads to:
- Atrophy: Glands shrink if oils aren’t released regularly (often due to incomplete blinking or chronic blockages).
- Rapid Tear Evaporation: A shortened Tear Break-Up Time (TBUT) causes dryness and irritation.
Aqueous Dry Eye: When Tears Are Insufficient
Aqueous-deficient dry eye occurs when the lacrimal glands don’t produce enough watery tears. Common causes include:
- Autoimmune conditions (e.g., Sjögren’s Disease, lupus).
- Medications (e.g., antihistamines, antidepressants).
- Aging or gland damage.
- Chronic dehydration (a key factor for many patients at our Seattle clinic).
Treating MGD vs. Aqueous Dry Eye: Custom Solutions for Lasting Relief
Recent studies show 86% of dry eye cases involve MGD, making it the most common culprit. Key causes include:
- Aging (reduced gland function).
- Blepharitis (eyelid inflammation).
- Excessive screen time (reduces blinking frequency).
- Incomplete blinking (we’ll cover this later!).
The Role of Meibomian Glands in Tear Health
Healthy meibomian glands produce oils that form the tear film’s lipid layer, preventing rapid evaporation.
When glands are clogged or blocked (often due to thickened oils), tear quality plummets, leading to:
- Faster tear evaporation (shortened TBUT).
- Intermittent blurry vision.
- Burning or gritty discomfort.
How SeattleEye Doctors Diagnose MGD
Your eye doctor can assess gland health by:
- Gentle Lid Compression: Checking for obstructions.
- Infrared Imaging: Advanced tools like those at Cannon EyeCare in Pike Place’s Market Optical capture detailed meibomian gland images.
Why Baseline Imaging Matters
- Track Changes: Annual imaging helps monitor gland atrophy.
- Insurance-Covered: Most plans cover this low-cost, non-invasive test.
Thermal Therapies for MGD & Dry Eye
Effective MGD treatment requires targeting two critical issues: gland obstruction and inflammation. Here’s how thermal therapies and expert care at Cannon EyeCare address these challenges:
Key Factors in MGD Treatment
-
Clearing Gland Obstructions
- Physical blockages in gland exit ports can stem from:
- Blepharitis (bacterial overgrowth on eyelids).
- Demodex mites infest lash follicles.
- Scarring from chronic inflammation or gland atrophy.
- External factors like eyeliner on the waterline or medications (e.g., Accutane) can also disrupt the lipid layer.
- Physical blockages in gland exit ports can stem from:
-
Reducing Inflammation
- Prevents scarring and further gland damage.
Why Early Treatment Matters
- Atrophy is irreversible: Once meibomian glands shrink from prolonged clogging, they can’t regenerate.
- Thermal Therapies + Gland Expression: Combining heat (to soften thickened oils) with manual gland clearing restores function in most cases.
How Eye Specialists Optimize Thermal Therapy
At Cannon EyeCare in Pike Place, Dr. Mark Cannon uses evidence-based protocols to:
- Melt obstructions: Heat applied to lids liquefies thickened oils.
- Express glands: Gentle pressure removes blockages, promoting healthy oil flow.
- Prevent recurrence: Customized lid hygiene plans reduce inflammation and scarring risks.
Critical Considerations for MGD Patients
- Avoid habits that worsen blockages (e.g., heavy eyeliner use).
- Address underlying issues like Demodex or blepharitis promptly.
- Annual imaging at our Pike Place clinic tracks gland health to guide adjustments in care.
Why Thermal Therapies Are Underused
Despite 87% of eye doctors agreeing that meibomian gland obstruction is central to MGD, only 5% of patients receive thermal therapies. This gap highlights a critical need for specialized care, which Cannon EyeCare in Seattle delivers through advanced in-office treatments.
The MGD Treatment Paradox: Awareness vs. Action
- 87% of providers recognize gland obstruction as a key issue.
- 71% advocate obstruction removal as the first treatment step.
- Yet, just 5% of patients receive thermal therapies.
Next-Level MGD Care: Thermal Gland Expression at Pike Place
Dr. Cannon’s approach includes:
- NuLids Device: Deep lid cleaning to remove debris and bacteria.
- Thermal Expression: Heating lids to melt blockages, followed by manual gland clearing.
- Post-Treatment Care: Non-preserved artificial tears, omega-3 supplements, or steroid drops (if needed) to reduce inflammation.
The Blinking Connection: How Incomplete Blinks Worsen Dry Eye
Your 50+ meibomian glands rely on proper blinking to release oils. A “good blink” involves:
- Full Lid Closure: Upper and lower lids touch completely.
- Gentle Pressure: Lids press together for ~1 second, wrinkling the lid margin.
- Oil Release: This “crumple” effect pumps oils into tears.
The Problem: Screen time, aging, or habits like partial blinking reduces oil secretion, accelerating tear evaporation.
For Seattle Patients: Proactive Dry Eye Solutions at Pike Place
At Cannon EyeCare, we prioritize:
- Thermal Expression Appointments: Advanced in-office relief for stubborn MGD.
- Blinking Retraining: Custom exercises to improve lid function.
- Annual Imaging: Track gland health with infrared technology.
Conclusion:
Understanding the difference between Meibomian Gland Dysfunction (MGD) and aqueous-deficient dry eye is the first step toward effective treatment. While MGD affects 86% of dry eye patients, only a small fraction receive targeted therapies like thermal gland expression—a gap Seattle’s Cannon EyeCare is closing with cutting-edge diagnostics and treatments.
Book a Comprehensive Dry Eye Evaluation: Visit Cannon EyeCare at Pike Place for advanced care.
FAQs
-
What is the main cause of evaporative dry eye?
Evaporative dry eye is primarily caused by Meibomian Gland Dysfunction (MGD), where clogged or damaged glands fail to produce healthy oils, leading to rapid tear evaporation.
-
How do I know if I have MGD or aqueous-deficient dry eye?
-
Can thermal therapies reverse gland atrophy?
-
Why choose Cannon EyeCare in Pike Place for MGD treatment?
-
How does blinking affect MGD?
-
Are warm compresses enough to treat MGD?
-
Will my insurance cover thermal gland expression?
-
What makes evaporative dry eye more common than aqueous-deficient?
-
How long does thermal therapy take to relieve symptoms?
-
Why is hydration important for dry eye?
-
Can I wear eyeliner if I have MGD?
-
Does screen time worsen MGD?
-
How often should I get meibomian gland imaging?
-
Will omega-3 supplements help my dry eye?
-
Are thermal therapies painful?



