Pinguecula vs. Pterygium: Causes, Symptoms & Treatment
Pinguecula vs. pterygium: Sun-damaged eye growths. Spot symptoms, prevent vision loss, and explore treatments. Protect your eyes from UV harm—essential insights inside.
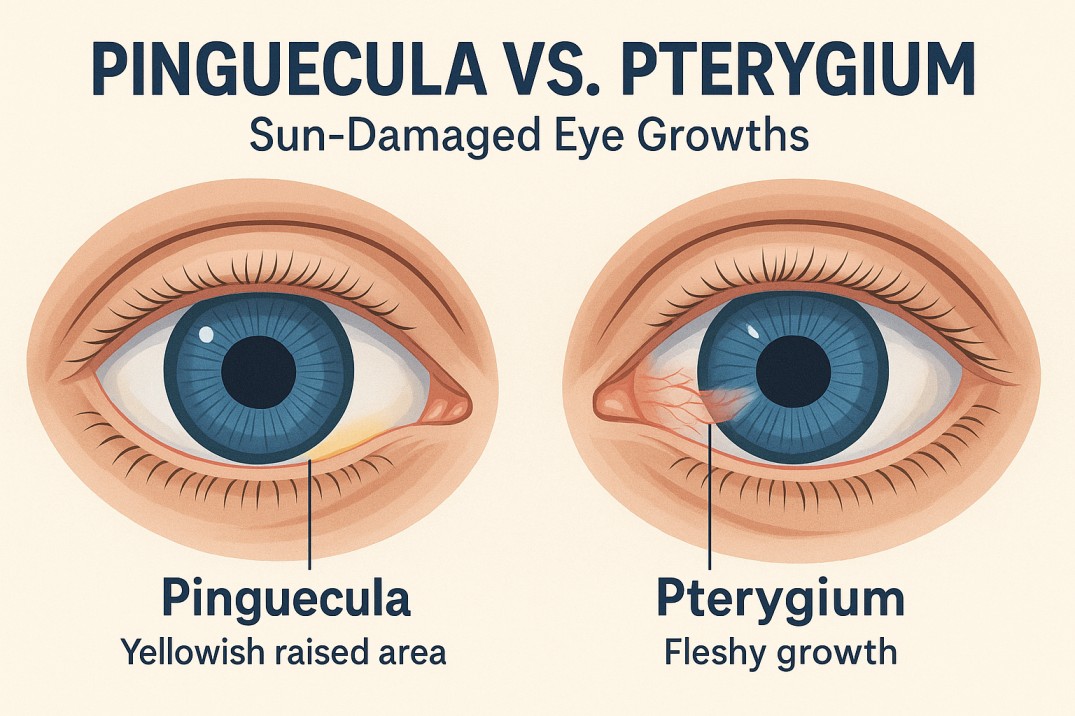
Characterized by a yellowish raised part of the scleral conjunctiva (the lining of the white part of the eye), a pinguecula usually develops near the cornea (colored part of the eye), but does not extend past it. Similar to a callus on the skin, changes in tissues lead to the buildup of calcium, fat, and/or protein, causing the bump or patch known as a pinguecula.
What is Pinguecula?
A pinguecula (pronounced pin-GWEK-yoo-la) is a common, benign growth that develops on the scleral conjunctiva, the thin, transparent membrane covering the white part of the eye (sclera).
Pinguecula Symptoms
A pinguecula causes a feeling of irritation – you may feel like something is caught in your eye. In some cases, a pinguecula leads to pingueculitis, a condition in which the pinguecula becomes swollen, irritated, and red. Often exposure to extreme dryness, wind, sun, or dust leads to pingueculitis. Wearing a hat and sunglasses while outdoors will help prevent pingueculitis.
Pinguecula Causes
The exact cause of pinguecula is not fully understood, but the condition has been associated with unprotected exposure to the sun’s ultraviolet rays.
Pinguecula Diagnosis and Treatment
An eye care professional can diagnose pinguecula with an examination, using a slit lamp to view the eye closely. Treatment depends on the severity of the symptoms present. Lubricating eye drops might be prescribed to relieve mild irritation, and if inflamed, either steroid eye drops or oral non-steroidal anti-inflammatory drugs. In severe cases, where the pinguecula interferes with blinking, vision, or contact lens wearing, surgical removal might be necessary.
Pterygium
Pingueculae often lead to the formation of pterygia, wedge-shaped growths elevated from the scleral conjunctiva, which grow past the cornea. Like pingueculae, pterygia are non-cancerous growths, but pterygia contain blood vessels and have the ability to permanently disfigure the eye, transforming its shape with scar tissue.
What is Pterygium?
A pterygium (pronounced tur-IH-jee-um) is a wedge-shaped, vascularized growth of conjunctival tissue that extends from the sclera onto the cornea. Unlike a pinguecula, it can impair vision if left untreated.
What is Surfer’s Eye?
Surfer’s eye is a colloquial term for pterygium, named for its high prevalence among surfers and others exposed to reflective UV rays from water, sand, or snow.
- Why the Name?
- Surfers, sailors, and fishermen are at high risk due to UV reflection off water, which intensifies sun exposure.
- UV radiation damages the conjunctiva, triggering abnormal tissue growth over time.
Pterygium Cause and Symptoms
A pterygium is spurred on by exposure to the sun and wind. For this reason, the condition is often referred to as surfer’s eye. Pterygia often cause a foreign body sensation and can become red and swollen. When a pterygium grows large enough, it can distort the shape of the eye, causing astigmatism and visual acuity problems.
Pterygium Diagnosis and Treatment
An eye care professional will make a diagnosis based on a close observation with a slit lamp. Pterygium treatment depends on the severity of symptoms, whether the pterygium is growing, and its causes. Mild cases can be treated with steroid eye drops. Severe cases require surgical removal, usually performed in the doctor’s office with local anesthetics. To prevent regrowth, an eye care provider might perform an autologous conjunctival autografting.
Pinguecula vs. Pterygium: Key Differences
Understanding the distinctions between pinguecula and pterygium is critical for accurate diagnosis and treatment. Below is a detailed breakdown of their unique characteristics:
- Appearance
- Pinguecula: Presents as a slightly raised, yellowish or white deposit on the scleral conjunctiva (white of the eye). It has a chalky or fatty texture and lacks blood vessels.
- Pterygium: A fleshy, triangular growth with visible red blood vessels. It often appears pink or red due to its vascular nature and may develop a “wing-like” shape as it advances.
- Location
- Pinguecula: Forms adjacent to the cornea (usually on the nasal or temporal side) but does not cross the limbus (the border between the cornea and sclera).
- Pterygium: Grows over the cornea, extending from the conjunctiva toward the pupil. This invasion can distort the corneal surface.
- Growth Pattern
- Pinguecula: Typically remains stable in size. While it may thicken slightly over time, it rarely progresses to cover the cornea.
- Pterygium: Progressive and invasive. If untreated, it can advance across the cornea, potentially obstructing the visual axis.
- Vascularization
- Pinguecula: Lacks blood vessels, making it less prone to inflammation.
- Pterygium: Contains blood vessels that supply the growth, contributing to redness, swelling, and irritation (especially during flare-ups).
- Symptoms
- Pinguecula: Often asymptomatic but may cause mild dryness, irritation, or a foreign-body sensation. Severe inflammation (pingueculitis) can occur with environmental triggers.
- Pterygium: More likely to cause persistent redness, blurred vision, and astigmatism. Advanced cases may lead to corneal scarring or vision loss.
- Treatment Urgency
- Pinguecula: Managed conservatively with lubricating drops, steroids for inflammation, or UV protection. Surgery is rare and reserved for severe discomfort.
- Pterygium: Requires proactive monitoring. Surgical removal is recommended if it grows >2mm into the cornea, distorts vision, or causes significant discomfort.
- Demographics
- Pinguecula: Most common in adults over 40, particularly those with a history of sun exposure or dry eye.
- Pterygium: Frequently seen in younger populations (ages 20–50), especially individuals in sunny, windy climates (e.g., surfers, farmers).
- Progression to Other Conditions
- Pinguecula: Does not transform into cancer but may act as a precursor to pterygium in some cases.
- Pterygium: While benign, untreated growths can permanently alter corneal shape and require complex surgical correction.
Prevention Strategies
Key Focus: Proactive measures to minimize risk and slow progression.
- UV Protection:
- Use wrap-around sunglasses with 100% UV protection (e.g., brands like Oakley or Ray-Ban with polarized lenses).
- UV-blocking contact lenses (e.g., Acuvue Oasys with Hydraclear) add an extra layer of defense.
- Wear wide-brimmed hats (3-inch brim or larger) to block overhead sunlight.
- Environmental Adjustments:
- Avoid outdoor activities during peak UV hours (10 AM–4 PM). Use protective goggles (e.g., Wiley X safety glasses) in dusty or windy conditions.
- Install car or workplace window UV filters to reduce incidental exposure.
- Nutritional Support:
- Omega-3 fatty acids (found in salmon, walnuts, and chia seeds) reduce dry eye symptoms by stabilizing the tear film.
- Stay hydrated (aim for 8–10 glasses of water daily) to maintain ocular surface moisture.
- Professional Monitoring:
- Schedule annual comprehensive eye exams with an optometrist or ophthalmologist to detect early changes.
Risk Factors
Key Focus: Identify populations and behaviors linked to higher incidence.
- Occupational Hazards:
- Outdoor workers (e.g., farmers, lifeguards) face 3x higher risk due to prolonged UV exposure.
- Athletes (e.g., cyclists, skiers) exposed to reflective UV rays from snow, water, or sand.
- Geographic Vulnerability:
- Residents of Australia, the Middle East, or equatorial regions have up to 20% higher prevalence.
- High-altitude areas (e.g., Andes Mountains) intensify UV radiation.
- Age and Health Status:
- Adults over 40 experience reduced tear production and collagen changes.
- Chronic conditions like rosacea or Sjögren’s syndrome exacerbate dry eye, accelerating pinguecula formation.
- Genetic Susceptibility:
- Family history increases risk by 15–20%, suggesting hereditary collagen or elastin degradation.
Differential Diagnosis
Key Focus: Distinguish from similar conditions to avoid misdiagnosis.
- Conjunctival Tumors:
- Squamous cell carcinoma presents as irregular, fast-growing masses; biopsy is mandatory.
- Melanoma shows pigmentation and requires urgent referral to an ocular oncologist.
- Limbal Dermoid:
- Congenital, hair-containing lesions diagnosed in childhood via ultrasound biomicroscopy.
- Conjunctival Cysts:
- Clear, fluid-filled sacs without vascularization; often resolve spontaneously.
- Diagnostic Tools:
- Slit lamp examination identifies lesion texture and vascular patterns.
- Anterior segment OCT maps lesion depth and corneal involvement.
Complications
Key Focus: Long-term consequences of untreated growths.
- Pinguecula Complications:
- Pingueculitis: Chronic inflammation causing redness, pain, and blurred vision.
- Dry Eye Syndrome: Disrupted tear film increases corneal abrasion risk.
- Pterygium Complications:
- Corneal Astigmatism: Growth-induced pressure distorts the cornea, leading to blurred vision.
- Vision Loss: If the pterygium encroaches the central cornea (visual axis), permanent scarring may occur.
Surgical Details and Recovery
Key Focus: Transparency about procedures and outcomes.
- Surgical Techniques:
- Excision with Conjunctival Autograft: Healthy tissue from under the eyelid is transplanted to prevent recurrence.
- Amniotic Membrane Grafting: Reduces inflammation and promotes healing in high-risk cases.
- Success Rates:
- Autografts reduce recurrence to 5–10% vs. 30–40% with bare sclera techniques.
- Post-surgery astigmatism correction improves vision in 70% of patients.
- Recovery Protocol:
- Week 1–2: Use prescribed steroid drops (e.g., prednisolone) 4x daily; avoid water exposure.
- Week 3–4: Gradual return to normal activities; monitor for redness or discharge.
Lifestyle Adjustments
Key Focus: Daily habits to manage symptoms and prevent flare-ups.
- Dry Eye Management:
- Apply preservative-free artificial tears (e.g., Systane Ultra, Refresh Optive) 4–6x daily.
- Use nighttime ointmentments (e.g., Refresh PM) to prevent nocturnal dryness.
- Environmental Modifications:
- Humidifiers (e.g., Honeywell HCM-350) maintain 40–60% indoor humidity.
- Avoid smoke, chlorine pools, and direct air conditioning drafts.
- Contact Lens Tips:
- Switch to daily disposables (e.g., Dailies Total1) to reduce protein deposits.
- Consider scleral lenses for irregular ocular surfaces post-surgery.
Prognosis and Long-Term Management
- Pinguecula:
- 90% remain stable with conservative care; monitor for growth every 6–12 months.
- Pterygium:
- 10–15% recurrence rate post-surgery; biannual exams are critical for early detection.
- Lifelong UV protection and lubricants reduce recurrence risk.
Home Remedies and OTC Options
Key Focus: Practical solutions for lens tolerance.
- Challenges:
- Pinguecula creates uneven lens fit, causing discomfort or displacement.
- Pterygium may warp the cornea, requiring frequent lens prescription updates.
- Solutions:
- Silicone hydrogel lenses (e.g., Air Optix Night & Day) improve oxygen flow.
- Prosthetic lenses mask irregular astigmatism in severe cases.
FAQs
-
What is the difference between a pinguecula and a pterygium?
A pinguecula is a yellowish, non-vascular bump on the sclera (white of the eye) near the cornea but doesn’t grow over it. A pterygium is a fleshy, triangular growth with blood vessels that extends onto the cornea, potentially affecting vision. While pingueculae rarely progress, pterygia can grow and require surgery.
-
How does UV exposure cause pinguecula and pterygium?
-
What symptoms indicate pingueculitis?
-
Can a pinguecula become a pterygium?
-
Why is a pterygium called “surfer’s eye”?
-
How does a pterygium affect vision?
-
What non-surgical treatments work for pinguecula?
-
When is surgery needed for a pterygium?
-
Who is most likely to develop a pinguecula?
-
Can contact lens wearers develop pinguecula?
-
What’s the recovery time after pterygium surgery?



