Diabetic Eye Exams: Essential Guide for Diabetes Patients
Why Regular Eye Screenings Can Save Your Vision
Quick Answer: If you have diabetes, annual dilated eye exams are essential—they’re the only way to detect diabetic retinopathy before it causes permanent vision loss. More than 90% of diabetes-related blindness is preventable with early detection.
Living with diabetes means your eyes face serious risks that many people don’t recognize until it’s too late. More than 90% of diabetes-related vision loss can be prevented with early detection and treatment, yet only about 60% of diabetes patients complete their recommended annual eye exams.
This comprehensive guide explains everything you need to know about diabetic eye exams and why they’re essential for protecting your sight.
Understanding Diabetic Eye Disease: What Every Patient Should Know
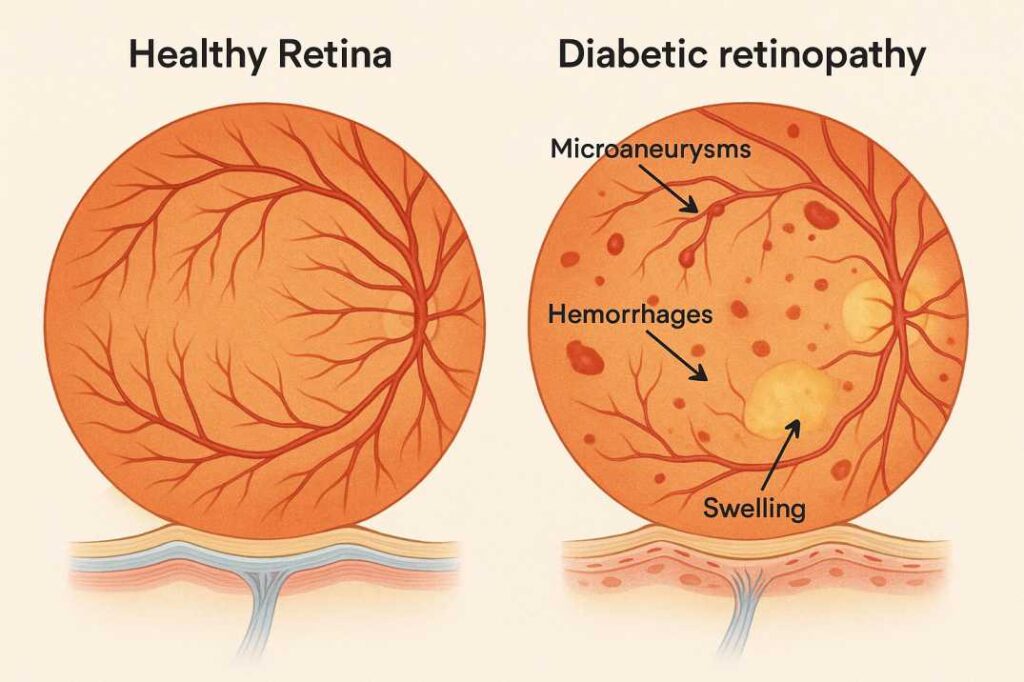
Diabetes doesn’t just affect your blood sugar—it can seriously damage your eyes. High glucose levels harm the tiny blood vessels in your retina, the light-sensitive tissue at the back of your eye that captures what you see. This damage often begins silently, with no symptoms or warning signs until significant vision loss occurs.
Diabetic retinopathy affects approximately 26% of people with diabetes in the United States (9.6 million Americans as of 2021) and stands as the leading cause of blindness among working-age adults in developed countries. The condition progresses through stages, starting with mild changes to blood vessels and potentially advancing to vision-threatening complications.
The Silent Nature of Early Eye Damage
The most dangerous aspect of diabetic eye disease is its stealth progression. You won’t feel pain. Your vision may seem perfectly normal. Yet beneath the surface, blood vessels are leaking, swelling, and deteriorating. By the time you notice blurry vision or floating spots, significant damage may have already occurred.
This is precisely why regular diabetic eye exams are non-negotiable—they’re your only defense against silent vision loss.
What Happens During a Comprehensive Diabetic Eye Exam
A diabetic eye exam goes far beyond a simple vision check. Your eye doctor conducts a thorough evaluation specifically focused on detecting diabetes-related complications before they threaten your sight.
The Essential Components
Visual Acuity Testing: Your doctor measures how clearly you see at various distances using the familiar eye chart with letters of different sizes. This establishes your baseline vision and identifies any changes since your last visit.
Dilated Eye Examination: This is the cornerstone of diabetic eye screening. Special eye drops widen your pupils, allowing your eye doctor to examine the entire retina, optic nerve, and blood vessels at the back of your eye. While the drops cause temporary blurred vision and light sensitivity for about 4-6 hours, this examination is essential for detecting early signs of retinopathy.
Intraocular Pressure Measurement: Your doctor checks the fluid pressure inside your eyes using a quick, painless test. Elevated pressure can signal glaucoma, which people with diabetes develop at nearly twice the rate of those without diabetes.
Retinal Photography: Many practices now use high-resolution cameras to capture detailed images of your retina. These photos create a permanent record, allowing your doctor to track even subtle changes over time and compare them with future visits.
Advanced Diagnostic Testing
When needed, your eye doctor may recommend additional tests:
Optical Coherence Tomography (OCT): This non-invasive imaging test creates cross-sectional pictures of your retina, revealing swelling, fluid leakage, or thinning that indicates diabetic macular edema or other complications.
Fluorescein Angiography: A special dye injected into your arm travels to your eye’s blood vessels, highlighting areas of damage, leakage, or abnormal blood vessel growth when photographed with a specialized camera.
How Often Do Diabetes Patients Need Eye Exams?
The timing of your diabetic eye exams depends on several factors, including your type of diabetes, how long you’ve had it, and whether any retinopathy has been detected.
Initial Screening Guidelines
Type 1 Diabetes: Schedule your first comprehensive eye exam within 3-5 years after diagnosis. Since Type 1 diabetes typically develops in childhood or adolescence and retinopathy rarely develops in the first few years, this timeline balances thoroughness with practicality.
Type 2 Diabetes: Get your first diabetic eye exam immediately upon diagnosis. Unlike Type 1, Type 2 diabetes often goes undiagnosed for years, meaning you may have already developed retinopathy without knowing it. Immediate screening catches existing problems and establishes your baseline.
Ongoing Monitoring Schedule
After your initial exam:
- Annual exams are standard for all diabetes patients with no retinopathy or only mild retinopathy
- Every 1-2 years may be acceptable if you’ve had multiple normal exams and your blood sugar is well-controlled
- Every 2-4 months or more frequently if retinopathy is progressing or you have diabetic macular edema
- Quarterly or more often if you’re receiving treatment for advanced diabetic eye disease
Special Circumstances Requiring More Frequent Exams
Pregnancy: Women with pre-existing diabetes who become pregnant need an exam as soon as pregnancy is confirmed or during the first trimester, then monitoring throughout pregnancy and for one year postpartum. Pregnancy can accelerate retinopathy progression due to hormonal changes and increased vascular stress.
Adolescence: Teenagers with diabetes require closer monitoring during puberty, when accelerated retinopathy progression commonly occurs.
Rapid Blood Sugar Changes: If you’re starting new diabetes medications that cause rapid glucose improvements (like GLP-1 receptor agonists, including semaglutide), your doctor may recommend more frequent eye monitoring, as rapid blood sugar normalization can temporarily worsen retinopathy.
The Most Common Diabetic Eye Conditions
Understanding what your eye doctor is screening for helps you recognize the importance of regular exams and stay alert to warning signs.
Diabetic Retinopathy: The Primary Concern
This condition occurs when high blood sugar damages the tiny blood vessels in your retina. It progresses through distinct stages:
Mild Nonproliferative Retinopathy: Small areas of swelling (microaneurysms) appear in retinal blood vessels. You’ll have no symptoms.
Moderate Nonproliferative Retinopathy: Blood vessels begin to swell and distort, and some become blocked, depriving parts of the retina of blood flow.
Severe Nonproliferative Retinopathy: Many blood vessels are blocked, causing significant areas of the retina to lose their blood supply. The retina signals for new blood vessel growth.
Proliferative Diabetic Retinopathy (PDR): New, abnormal blood vessels grow on the retina’s surface and into the vitreous gel, filling your eye. These fragile vessels leak easily, causing vision-threatening bleeding, scar tissue, and potential retinal detachment.
Diabetic Macular Edema (DME)
This complication can develop at any stage of retinopathy when fluid accumulates in the macula—the central part of your retina responsible for sharp, detailed vision. DME causes blurred central vision and is a leading cause of vision loss in diabetes patients.
Additional Diabetes-Related Eye Conditions
Cataracts: People with diabetes develop cloudy lenses 2-5 times more often than those without diabetes, and at younger ages. Cataracts cause progressively blurred vision, glare, and difficulty seeing at night.
Glaucoma: Diabetes nearly doubles your risk of glaucoma, a group of conditions where increased eye pressure damages the optic nerve. Often symptomless until advanced stages, glaucoma causes irreversible vision loss if untreated.
Retinal Vessel Occlusions: Diabetes increases the risk of blood clots blocking retinal arteries or veins, causing sudden, painless vision loss.
How Can I Protect My Eyes If I Have Diabetes?
The best protection combines regular dilated eye exams (annually or as recommended), excellent blood sugar control (HbA1c below 7%), blood pressure management (under 140/90), and healthy lifestyle choices, including not smoking, regular exercise, and a diabetes-friendly diet. Early detection through annual screenings prevents 90% of vision loss.
Warning Signs That Require Immediate Attention
While diabetic eye disease often progresses without symptoms, certain changes demand urgent evaluation:
- Sudden vision changes – Rapid blurring, vision loss, or distortion
- Floaters – New dark spots, strings, or cobwebs drifting across your vision
- Flashes of light – Sudden, brief streaks or flashes, especially in peripheral vision
- Curtain or shadow – A dark area blocking part of your visual field
- Eye pain or redness – Unusual discomfort, especially with vision changes
- Difficulty seeing at night – Worsening night vision or increased glare sensitivity
Don’t wait for your scheduled appointment if you experience any of these symptoms. Contact your eye doctor immediately or seek emergency care—these could indicate serious complications requiring urgent treatment.
Preparing for Your Diabetic Eye Exam: A Complete Checklist
Maximize the value of your appointment with thorough preparation:
Information to Gather
- Your diabetes history – Date of diagnosis, type of diabetes, recent A1C levels (last 3-6 months), current and past diabetes medications
- Blood sugar logs – Recent readings showing how well your diabetes is controlled
- Complete medication list – All prescriptions, over-the-counter drugs, vitamins, and supplements with dosages
- Eye symptom journal – Notes on any vision changes, when they occur, and what triggers or relieves them
- Family eye health history – Glaucoma, cataracts, or other eye conditions in blood relatives
- Other health conditions – Blood pressure, cholesterol levels, kidney disease, cardiovascular problems
What to Bring
- All corrective eyewear – Current glasses and contact lenses
- Sunglasses – Essential for the drive home after pupil dilation
- Insurance cards – Both medical and vision insurance
- A driver – You cannot safely drive for 4-6 hours after dilation
- Questions list – Write down concerns or questions beforehand so you don’t forget
Plan Your Day Around the Appointment
- Schedule adequate time: Eye exams with dilation typically take 1-2 hours, including wait time
- Bring snacks: If you have Type 1 diabetes or use insulin, bring fast-acting carbohydrates to prevent hypoglycemia during the wait
- Clear your schedule: Don’t plan to read, use computers, or do detailed work for several hours after the exam
- Arrange transportation: Have someone drive you, use a rideshare service, or take public transit
Understanding Your Eye Exam Results and Next Steps
Your eye doctor will explain findings in terms of retinopathy grading and recommendations for follow-up or treatment.
The Diabetic Retinopathy Severity Scale
Eye doctors use standardized classifications:
- No apparent retinopathy: No signs of diabetes-related eye damage
- Mild nonproliferative: Microaneurysms only
- Moderate nonproliferative: More than just microaneurysms but less than severe
- Severe nonproliferative: Extensive hemorrhages, microaneurysms, or venous beading without proliferative disease
- Proliferative diabetic retinopathy: New abnormal blood vessel growth
Maculopathy Assessment
Your macula will be assessed separately:
- No maculopathy: No swelling or exudates affecting the macula
- Maculopathy present: Swelling, hard exudates, or other changes affecting central vision
What Your Results Mean for Treatment
No retinopathy or mild changes: Continue annual exams, focus on blood sugar control, maintain healthy lifestyle habits.
Moderate nonproliferative retinopathy: More frequent monitoring (every 6-12 months), intensified diabetes management, possible referral to retina specialist.
Severe nonproliferative or proliferative retinopathy: Immediate referral to a retina specialist, treatment planning, and very frequent monitoring.
Diabetic macular edema: Treatment is typically recommended regardless of retinopathy stage; options include anti-VEGF injections, steroid injections, or laser therapy.
Treatment Options for Diabetic Eye Disease
Modern treatments can prevent vision loss or even improve vision when started promptly.
Anti-VEGF Injections
These medications block vascular endothelial growth factor (VEGF), a protein that stimulates abnormal blood vessel growth and increases vascular permeability. Drugs like ranibizumab, aflibercept, and bevacizumab are injected directly into the eye to:
- Reduce retinal swelling from diabetic macular edema
- Shrink abnormal blood vessels in proliferative retinopathy
- Prevent disease progression
- Improve vision in many cases
Treatment involves regular injections—initially monthly, then potentially extending to every 2-3 months depending on your response.
Laser Photocoagulation
Focal/Grid Laser: Precisely targets leaking blood vessels in the macula to reduce swelling from diabetic macular edema.
Panretinal Photocoagulation (PRP): Creates thousands of tiny burns in the peripheral retina, reducing oxygen demand and preventing abnormal blood vessel growth in proliferative retinopathy. While effective at preventing vision loss, PRP may cause some peripheral vision reduction and night vision difficulties.
Steroid Treatments
Corticosteroid injections or implants reduce inflammation and vascular permeability. Options include triamcinolone injections or longer-lasting implants like dexamethasone (Ozurdex) or fluocinolone (Iluvien). These are typically reserved for cases where anti-VEGF therapy isn’t sufficient or feasible.
Surgical Options
Vitrectomy: This surgical procedure removes blood-filled vitreous gel and scar tissue, repairs retinal detachments, and clears the visual pathway when bleeding or scarring severely impairs vision.
Emerging Therapies
Recent advances include longer-acting formulations, port delivery systems that reduce injection frequency, and novel drug targets beyond VEGF. Clinical trials are investigating oral medications, topical treatments, and gene therapies that may revolutionize diabetic eye disease treatment in the coming years.
The Critical Connection: Blood Sugar Control and Eye Health
Your blood sugar management directly impacts your eye health and determines your retinopathy risk more than any other factor.
Research-Backed Benefits of Glycemic Control
Landmark studies prove that maintaining HbA1c below 7% can:
- Reduce retinopathy risk by 76% in Type 1 diabetes (DCCT study)
- Slow retinopathy progression by 25% in Type 2 diabetes (UKPDS study)
- Decrease severe vision loss risk by 50% with sustained control
Beyond Blood Sugar: Other Protective Factors
Blood Pressure Management
Maintaining blood pressure below 140/90 mmHg (or targets set by your doctor) significantly reduces retinopathy progression. The combination of glucose and blood pressure control provides additive protection.
Cholesterol Control
Managing lipid levels, particularly with fenofibrate in some studies, shows promise in slowing diabetic retinopathy progression.
Healthy Lifestyle Choices
- Regular physical activity improves circulation and glucose control
- Mediterranean-style diet rich in vegetables, fish, and healthy fats
- Smoking cessation (smoking worsens diabetic eye disease)
- Maintaining a healthy body weight
A Word of Caution: Avoid Rapid Blood Sugar Changes
While excellent glucose control protects your eyes long-term, rapid normalization of previously high blood sugar can temporarily worsen retinopathy. This “early worsening phenomenon” occurs when HbA1c drops more than 2% within 3-6 months.
If you’re starting intensive diabetes treatment or new medications causing rapid glucose improvements, your doctor should monitor your eyes more frequently during this transition period.
Insurance Coverage and Financial Considerations for Diabetic Eye Exams
Understanding coverage helps you get necessary care without financial barriers.
Medicare Coverage
Medicare Part B covers diabetic eye exams once yearly for all beneficiaries with diabetes. After meeting your Part B deductible ($257 in 2025), you pay 20% of the Medicare-approved amount. The exam must be performed by an ophthalmologist or optometrist.
Private Insurance
Most private health insurance plans cover diabetic eye exams as preventive care, often with:
- Annual coverage without prior authorization
- Covered under medical benefits (not vision plans)
- Minimal or no copay for in-network providers
- Possible coverage for screening photography or specialized testing
Check your specific plan for:
- In-network vs. out-of-network provider costs
- Frequency limits
- Prior authorization requirements for specialized testing
- Coverage for treatment procedures if retinopathy is detected
Medicaid
Diabetic eye exam coverage varies by state, but generally includes:
- Routine diabetic screening exams
- Diagnostic testing is medically necessary
- Treatment procedures for diabetic retinopathy
- Often, with minimal or no out-of-pocket costs for recipients
For Uninsured Patients
If you don’t have insurance:
- Community health centers often provide sliding-scale fee services
- EyeCare America offers free eye exams for eligible seniors through the American Academy of Ophthalmology
- Lions Clubs International may assist with eye care costs
- Pharmaceutical company patient assistance programs can help with treatment medication costs
- Local diabetes organizations sometimes offer screening events
- Payment plans – Ask about payment plans at your eye doctor’s office
Innovative Technologies Transforming Diabetic Eye Screening
Advances in technology are making diabetic eye exams more accessible, accurate, and convenient.
Artificial Intelligence (AI) Screening Systems
FDA-approved AI platforms can now detect diabetic retinopathy with accuracy comparable to human experts:
How It Works: A specially trained technician takes retinal photographs without dilating your pupils. The AI system analyzes images in minutes, determining whether diabetes-related eye disease is present and whether referral to an eye specialist is needed.
Advantages:
- No dilation required (no vision disruption)
- Results are often available the same day
- Can be offered in your primary care doctor’s office
- Improves screening rates, especially for underserved populations
- May reduce overall healthcare costs
Current FDA-approved systems include IDx-DR (Digital Diagnostics), EyeArt (Eyenuk), and AEYE-DS (AEYE Health). A 2024 Johns Hopkins study found AI screening increased youth diabetes eye exam rates from 22% to 100% when offered at the point of care.
Teleophthalmology Programs
Remote screening allows retinal imaging at one location with expert evaluation performed elsewhere:
- Cameras capture fundus photographs
- Images transmitted securely to reading centers
- Ophthalmologists or certified graders evaluate remotely
- Results and recommendations are returned to your doctor, and you
- Particularly valuable for rural or underserved areas
Studies show teleophthalmology sensitivity of 62.5-98.2% and specificity of 76.6-98.7% for detecting referable diabetic retinopathy—comparable to in-person exams.
Ultra-Widefield Imaging
Traditional retinal cameras capture about 30-50 degrees of the retina. Ultra-widefield systems photograph up to 200 degrees (82% of the retinal surface) in a single image, revealing:
- Peripheral retinopathy lesions that predict progression risk
- More complete disease assessment
- Better monitoring of treatment response
- Improved patient education through comprehensive visual documentation
Optical Coherence Tomography Angiography (OCTA)
This non-invasive technology visualizes retinal blood flow at the capillary level without injecting dye:
- Reveals microvascular changes invisible on standard exams
- Quantifies areas of reduced blood flow (ischemia)
- Assesses macular health in fine detail
- Tracks treatment response precisely
OCTA is revolutionizing our understanding of diabetic eye disease progression and treatment mechanisms.
Special Populations: Tailored Screening Recommendations
Certain groups require modified screening approaches:
Children and Adolescents with Diabetes
Youth with Type 1 Diabetes:
- First exam 3-5 years after diagnosis (once age 10 or older)
- More frequent monitoring during puberty due to accelerated progression risk
- AI screening showing promise for improving adherence rates in this age group
Youth with Type 2 Diabetes:
- First exam at diagnosis or shortly after
- Often have had diabetes longer than realized before diagnosis
- Higher baseline retinopathy rates than Type 1 youth of the same diabetes duration
Pregnant Women with Pre-Existing Diabetes
Pregnancy significantly affects diabetic retinopathy risk due to:
- Hormonal changes affecting vascular stability
- Increased blood volume and pressure
- Rapid glucose improvements are often implemented at conception
Screening Schedule:
- Exam before conception or within the first trimester
- Follow up each trimester
- Continued monitoring for 12 months postpartum
Important Note: Women who develop gestational diabetes (diabetes arising during pregnancy) without pre-existing diabetes do not require retinopathy screening, as they’re not at increased risk during pregnancy.
Older Adults (65+)
Seniors often face unique challenges:
- Higher prevalence of cataracts and glaucoma complicating diabetic screening
- Multiple chronic conditions requiring care coordination
- Transportation difficulties for medical appointments
- Cognitive changes affecting self-care and appointment adherence
Solutions include:
- Home-based AI screening when available
- Coordinated care appointments combining multiple specialties
- Transportation assistance programs
- Simplified treatment regimens when appropriate
Global Perspective: Diabetic Eye Disease Burden and Screening Programs
Diabetic retinopathy is a worldwide public health crisis with significant geographic disparities.
The Growing Global Challenge
- Over 100 million people worldwide live with diabetic retinopathy
- 16 million people in the U.S. are projected to have diabetic retinopathy by 2050
- Shifting burden: Increasing prevalence in low- and middle-income countries as diabetes rates rise
- Economic impact: Billions in healthcare costs and lost productivity
Screening Program Success Stories
United Kingdom: The National Health Service Diabetic Eye Screening Programme, established in 2003, achieved dramatic results. For the first time in 50 years, diabetic retinopathy was no longer the leading cause of blindness in working-age adults.
Iceland: A comprehensive national screening program with centralized grading and systematic recall achieves over 85% screening participation.
Singapore: Integrated screening with primary care and widespread use of AI and telemedicine reaching diverse populations.
Implementation Challenges
Many countries struggle with:
- Limited ophthalmology workforce, particularly in rural areas
- Inadequate retinal imaging equipment
- Poor integration between diabetes care and eye care systems
- Low patient awareness and screening uptake
- Financial barriers to accessing care
Future Directions
The WHO and international organizations are working toward:
- Universal screening access through telemedicine and AI
- Standardized classification systems globally
- Integration of screening into diabetes care pathways
- Training programs for mid-level eye care providers
- Cost-effective screening strategies for resource-limited settings
Taking Action: Your Eye Health Protection Plan
Protecting your vision from diabetes requires a proactive, comprehensive approach:
Immediate Steps
- Schedule your eye exam if overdue – Don’t delay another day
- Compile your medical information using the preparation checklist above
- Review your insurance coverage to understand costs and in-network providers
- Arrange transportation for after your dilated exam
Ongoing Prevention Strategy
- Maintain target blood sugar levels – Work with your diabetes care team to achieve HbA1c goals
- Control blood pressure and cholesterol – These factors compound the effects of diabetes on the eyes
- Attend all scheduled eye exams – Set automatic reminders; treat appointments as non-negotiable
- Adopt protective daily habits:
- Take prescribed diabetes medications consistently
- Follow a diabetes-friendly eating plan
- Exercise regularly (at least 150 minutes weekly)
- Don’t smoke; quit if you currently smoke
- Wear sunglasses outdoors for UV protection
- Monitor for warning signs – Check your vision regularly; report changes immediately
- Coordinate care – Ensure your eye doctor and diabetes doctor communicate about your health
- Stay informed – Learn about new treatments and screening options
Building Your Support System
- Connect with diabetes support groups – Share experiences and learn from others.
- Involve family members – Educate loved ones about warning signs and your appointment schedule.
- Work with diabetes educators – They provide valuable guidance on disease management.
- Use technology – Apps can help track appointments, glucose levels, and medication schedules.s
- Communicate openly with your healthcare team – Ask questions, express concerns, report barriers to care.
Research Foundation: Scientific Studies Supporting Diabetic Eye Care
This guide is informed by extensive peer-reviewed research and clinical guidelines:
Recent Clinical Studies (2024-2025)
1. AI-Enhanced Screening Effectiveness (Wolf et al., Nature Communications, 2024)
- Demonstrated that autonomous artificial intelligence screening increased diabetic retinopathy exam rates from 22% to 100% in youth with diabetes
- Point-of-care AI screening eliminated barriers related to scheduling separate appointments.
- No disparities in screening completion based on race, gender, or socioeconomic status
- Link: https://www.nature.com/articles/s41467-023-44676-z
2. Twenty-Year Trends in Diabetic Retinal Disease (Ophthalmology, January 2025)
- Large-scale longitudinal analysis showing shifting prevalence and incidence patterns of diabetic retinopathy
- Identified demographic and clinical factors associated with disease progression
- Emphasized the importance of sustained screening programs
- Link: https://www.aaojournal.org/article/S0161-6420(25)00076-4/fulltext
3. American Diabetes Association 2025 Standards of Care (Diabetes Care, January 2025)
- Updated comprehensive guidelines for diabetic retinopathy screening and management
- Evidence-based recommendations for screening frequency based on diabetes type and retinopathy status
- Integration of newer technologies, including AI and teleophthalmology
- Link: https://diabetesjournals.org/care/article/48/Supplement_1/S252/157552
Guidelines and Systematic Reviews
These recommendations align with:
- American Academy of Ophthalmology Diabetic Retinopathy Preferred Practice Pattern (2024-2025)
- International Council of Ophthalmology Guidelines for Diabetic Eye Care
- American Diabetes Association Clinical Practice Recommendations
- UK National Health Service Diabetic Eye Screening Programme protocols
- WHO guidance on diabetic retinopathy screening programs
Key Resources and Citations
Essential Guidelines and Standards
1. American Diabetes Association – 2025 Standards of Care in Diabetes
The most current clinical practice guidelines for diabetic retinopathy screening and management.
Link: https://diabetesjournals.org/care/article/48/Supplement_1/S252/157552/12-Retinopathy-Neuropathy-and-Foot-Care-Standards
2. American Academy of Ophthalmology – Diabetic Retinopathy Preferred Practice Pattern (2025)
Evidence-based recommendations for screening frequency, examination techniques, and treatment protocols.
Link: https://www.aao.org/education/preferred-practice-pattern/diabetic-retinopathy-ppp
3. Centers for Disease Control and Prevention – Vision and Eye Health Surveillance
Current U.S. prevalence data and diabetic retinopathy statistics (updated 2025).
Link: https://www.cdc.gov/vision-health-data/prevalence-estimates/dr-prevalence.html
4. National Eye Institute – Diabetic Retinopathy Information
Patient education resources on diabetic eye disease prevention and treatment.
Link: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
5. Medicare.gov – Eye Exams for Diabetes Coverage
Official information on Medicare Part B coverage for diabetic eye exams.
Link: https://www.medicare.gov/coverage/eye-exams-for-diabetes
Conclusion: Your Vision Is Worth Protecting
Bottom Line: Annual dilated eye exams are your most powerful defense against diabetic blindness. Book your exam today if you haven’t had one in the past year—early detection saves vision.
Diabetic eye disease threatens one of your most precious senses, but it doesn’t have to rob you of sight. Regular comprehensive eye exams provide the early warning system you need to catch problems before they cause permanent damage.
Remember these essential facts:
- Early diabetic retinopathy has no symptoms—you cannot rely on how your vision feels
- More than 90% of diabetes-related vision loss is preventable with timely detection and treatment
- Annual eye exams are your most powerful protection against blindness from diabetes
- Treatment works best when started early—don’t wait until vision problems develop
- Your blood sugar control directly impacts your eye health—every day of good management protects your sight
The relationship between diabetes care and eye health is crystal clear: dedicated disease management combined with regular professional eye screening gives you the best possible chance of maintaining healthy vision for life.
Your next step is simple: If you haven’t had a dilated eye exam within the past year, schedule one today. This single action could be the difference between a lifetime of clear vision and preventable blindness.
About Cannon EyeCare: Your Seattle Partner in Diabetic Eye Health
At Cannon EyeCare, we bring together advanced diabetic eye screening technology with the genuine, unhurried care our Seattle patients deserve. Located in University Village and Pike Place Market, our practice combines comprehensive medical expertise with Midwestern hospitality.
Our Diabetic Eye Care Approach
We understand that living with diabetes means managing multiple health priorities. That’s why we’ve designed our diabetic eye care services to be thorough yet convenient, using state-of-the-art diagnostic equipment to catch problems early while taking time to explain findings in clear, understandable terms.
Our Services Include:
- Comprehensive dilated eye examinations for diabetes patients
- Advanced retinal imaging and OCT scanning
- Early detection screening for diabetic retinopathy, macular edema, glaucoma, and cataracts
- Care coordination with your diabetes treatment team
- Same-day urgent appointments available
- Convenient scheduling with evening and weekend options
- Insurance verification assistance for Medicare, Premera, Regence, Kaiser PPO, and most major plans
Why Choose Cannon EyeCare for Your Diabetic Eye Exams
Thorough Excellence: We never rush. Every exam receives the time and attention needed to catch issues other providers might miss.
Genuine Personal Connection: We build lasting relationships with our patients, remembering not just your medical history but what matters in your life.
Convenient Seattle Locations:
- University Village: Easy access with ample parking
- Pike Place Market: Downtown convenience for city professionals
Specialized Expertise: Our doctors have specific training in diabetic eye disease management and work closely with endocrinologists and primary care providers throughout Seattle.
Schedule Your Diabetic Eye Exam
Whether you’re newly diagnosed with diabetes, overdue for your annual screening, or experiencing vision changes, we’re here to help protect your sight.
We accept most major insurance plans and will verify your coverage before your appointment. Our team is happy to answer questions about costs, insurance, and what to expect during your visit.
FAQs
-
-
A diabetic eye exam is a special eye check to spot early signs of diabetes-related damage, protecting vision for people with diabetes.
-