Diabetic Retinopathy: What Is It?
Diabetic retinopathy (DR) is an eye condition caused by damage to the small blood vessels in the retina and is a leading cause of vision loss and blindness in people with diabetes, making regular eye exams essential for prevention and early treatment. Early-stage DR often has no symptoms, so annual comprehensive dilated eye exams are critical even when vision seems normal to catch changes before they threaten sight. The risk of DR grows with the duration of diabetes and poor control of blood sugar, blood pressure, and lipids, but proactive care and timely treatment can prevent or delay vision loss for most patients. In the U.S., recent modeling indicates millions live with DR, underscoring the importance of screening and control in every community, including Seattle’s diverse population served by local eye care providers and retina specialists.
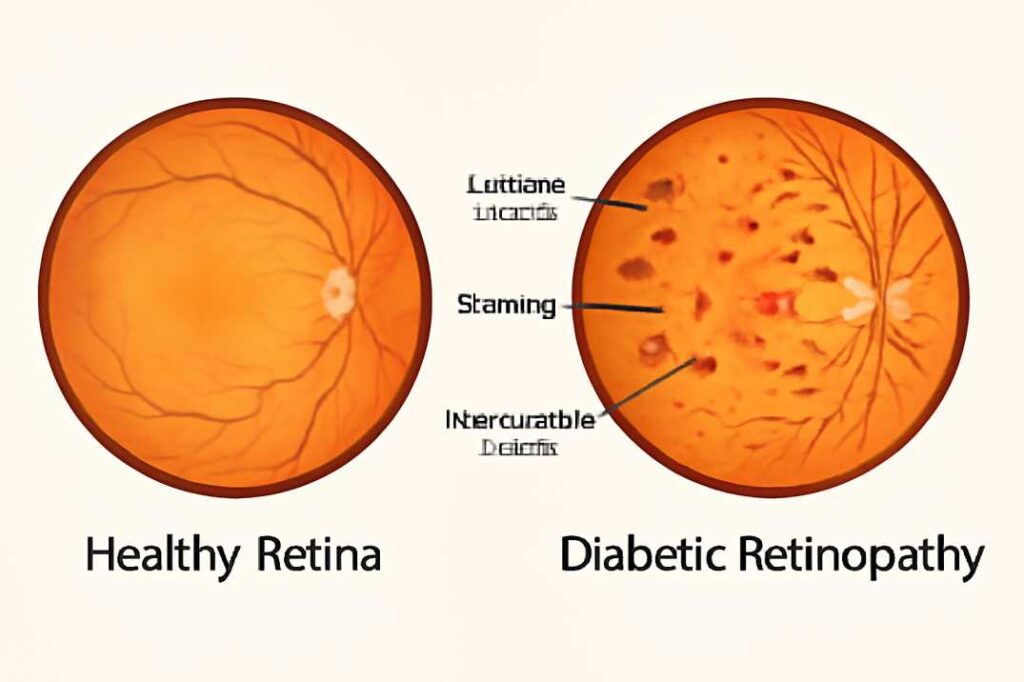
What Is Diabetic Retinopathy?
Diabetic retinopathy is a serious eye disease caused by diabetes that damages the blood vessels in the retina. This condition often begins with mild, symptom-free changes but can progress to severe, vision-threatening complications. These include macular edema (swelling), bleeding inside the eye, and retinal detachment.
There are two main types:
-
Nonproliferative Diabetic Retinopathy (NPDR): The early stage where abnormal new blood vessels have not yet formed.
-
Proliferative Diabetic Retinopathy (PDR): The advanced stage where fragile, new blood vessels grow. These can leak blood or cause scar tissue that pulls on the retina.
A major cause of vision loss from this disease is Diabetic Macular Edema (DME), which is swelling in the central part of the retina (the macula). DME can develop at any stage and often requires specialized treatment to protect your central vision. If you have diabetes in the Seattle area, regular comprehensive eye exams at Cannon EyeCare are your best defense against diabetic retinopathy.
Who is at Risk for Diabetic Retinopathy? Key Factors to Know
Anyone with type 1 or type 2 diabetes can develop diabetic retinopathy. Your risk increases significantly based on several key factors:
-
Duration of Diabetes: The longer you have had diabetes, the greater your risk.
-
Poor Blood Sugar Control: Consistently high blood sugar levels, measured by an elevated A1C, is a primary driver of the disease. Managing your A1C is one of the most critical steps in protecting your vision.
-
High Blood Pressure & Cholesterol: These conditions can accelerate damage to the retina’s delicate blood vessels.
-
Other Health Factors: Kidney disease (nephropathy), tobacco use, and pregnancy also substantially increase risk.
Certain populations face a disproportionately higher rate of vision-threatening diabetic retinopathy, underscoring the need for accessible, equity-focused eye care.
Nationally, diabetic retinopathy is a leading cause of blindness. Recent estimates show:
-
9.6 million people in the U.S. have diabetic retinopathy.
-
1.84 million people have reached the vision-threatening stage.
Diabetic Retinopathy Symptoms: When to See an Eye Doctor
In its earliest stages, diabetic retinopathy often has no symptoms whatsoever. Relying on vision alone is risky, as permanent damage can occur before you notice any changes.
As the disease progresses, you may experience:
-
Blurred or fluctuating vision
-
Increasing dark spots or floaters in your field of view
-
Areas of your vision that feel dim or missing
-
Gradual vision loss
These symptoms require a prompt, comprehensive eye exam to check for conditions like macular edema or bleeding.
Seek Urgent Care Immediately if you experience:
-
A sudden shower of new floaters
-
Flashes of light in your vision
-
A dark, curtain-like shadow across your sight
-
A sudden, dramatic drop in vision
These are emergency warning signs of a retinal detachment or significant vitreous hemorrhage, which can lead to permanent vision loss without swift treatment.
How Diabetic Retinopathy Develops: A Simple Explanation
Diabetic retinopathy begins with consistently high blood sugar levels, which act as a slow poison to the delicate blood vessels in your retina. This process unfolds in a few key stages:
-
The Initial Damage: Chronically high glucose triggers harmful inflammation and several complex biochemical pathways inside the retina. These processes (with long names like the polyol pathway and advanced glycation end-products) collectively damage the tiny capillaries, injuring the retina’s essential “neurovascular unit.”
-
Leakage and Blockages: The damaged vessel walls become weak and start to leak fluid and blood (a condition called edema). Simultaneously, other vessels can become blocked, starving areas of the retina of vital oxygen and nutrients.
-
Abnormal New Growth: In response to this oxygen starvation (ischemia), the eye panics and tries to grow new blood vessels to fix the problem—this is the start of Proliferative Diabetic Retinopathy (PDR). However, these new vessels are extremely fragile, defective, and prone to sudden bleeding or forming scar tissue that can pull on the retina.
Other Risk Factors: High blood pressure and cholesterol significantly worsen this vascular injury, which is why comprehensive management of all your health numbers—not just your A1C—is crucial for slowing the disease’s progression.
A Note on Vision Changes: It’s important to know that some temporary vision blur after rapid sugar changes is often due to swelling in the eye’s lens, which can improve as your levels stabilize. However, structural damage to the retina heals much more slowly and may require specific medical treatments. This distinction helps set realistic expectations on your journey to getting back on track.
How is Diabetic Retinopathy Diagnosed? The Essential Tests Explained
Diagnosing diabetic retinopathy requires a thorough, painless eye exam to see the detailed structures of your retina. At Cannon EyeCare in Seattle, we use the most advanced technology to accurately detect and stage the disease. Here are the key tests you can expect:
-
Comprehensive Dilated Eye Exam: This is the cornerstone of diagnosis. We use special drops to widen your pupils, allowing our doctors to get a clear, wide-angle view of your retina. This exam detects the hallmark signs of DR, including:
-
Microaneurysms: Tiny bulges in blood vessels.
-
Hemorrhages: Small spots of bleeding.
-
Exudates: Leaked fatty deposits.
-
Neovascularization: The growth of abnormal, fragile new blood vessels.
-
-
Optical Coherence Tomography (OCT): This advanced imaging test is crucial. It acts like a microscopic ultrasound, creating detailed cross-sectional images of your retina. The OCT is essential for:
-
Diagnosing and precisely measuring macular edema (DME).
-
Monitoring your retina’s response to treatment over time.
-
-
Angiography (FA or OCTA): For a deeper look at blood flow, we may recommend an angiogram.
-
Fluorescein Angiography (FA): A safe dye is injected into a vein in your arm, and as it travels through the blood vessels in your retina, a special camera highlights areas of leakage or poor circulation (ischemia).
-
OCT Angiography (OCTA): This newer technology maps blood flow in the retina without the need for any injections, providing detailed 3D images of the microvasculature.
-
These imaging tools are foundational. They provide the critical data our specialists need to make precise decisions about the timing and type of treatment—whether that’s injections, laser, or surgery.
Understanding the Stages of Diabetic Retinopathy: NPDR, PDR, and DME
Diabetic retinopathy progresses through distinct stages, each with specific characteristics and treatment goals. Understanding these stages helps clarify your diagnosis and the rationale behind your treatment plan at Cannon EyeCare.
1. Nonproliferative Diabetic Retinopathy (NPDR)
This is the early stage of the disease, where existing blood vessels in the retina become damaged. They may weaken, bulge (microaneurysms), leak fluid or blood (hemorrhages), or close off. NPDR is categorized by severity:
-
Mild to Moderate NPDR: Early signs are present, but vision is often still normal.
-
Severe NPDR: Significant vessel damage and closure occur, greatly increasing the risk of progressing to the advanced stage. Regular monitoring is crucial.
2. Proliferative Diabetic Retinopathy (PDR)
This is the advanced stage. In response to oxygen starvation (ischemia), the retina grows fragile, abnormal new blood vessels (neovascularization). These vessels are defective and can:
-
Leak blood into the vitreous gel of the eye (vitreous hemorrhage), causing sudden floaters or vision loss.
-
Form scar tissue that can pull on the retina and cause a tractional retinal detachment, a serious sight-threatening emergency.
Treatment for PDR focuses on making these abnormal vessels regress to prevent these catastrophic events.
3. Diabetic Macular Edema (DME)
DME can occur at any stage of NPDR or PDR. It happens when leaky vessels cause fluid to accumulate in the macula—the central part of the retina responsible for sharp, detailed vision. This swelling causes blurred central vision.
-
Center-Involving DME: When the swelling affects the very center of the macula. This is typically treated with anti-VEGF injections as a first-line therapy to reduce leakage and swelling.
In summary, the disease burden rests on three key problems, as summarized by EyeWiki:
-
Capillary Leakage: Causing edema (swelling).
-
Capillary Occlusion: Causing areas of poor blood flow (ischemia).
-
Ischemic Sequelae: The damaging consequences of ischemia, like abnormal blood vessel growth.
Diabetic Retinopathy Treatments: A Guide to Injections, Laser, and Surgery
Managing diabetic retinopathy involves advanced, targeted treatments to preserve your vision. At Cannon EyeCare in Seattle, we create personalized plans based on the specific stage and complications of your disease. Here’s what you can expect from modern treatment options.
1. Anti-VEGF Injections (First-Line Treatment for DME and PDR)
These medicated injections are a cornerstone of treatment. They work by blocking a protein that causes leaky vessels and abnormal growth.
-
Common Medications: Aflibercept (Eylea®), Ranibizumab (Lucentis®), and Bevacizumab (Avastin®). Newer, advanced options like Faricimab (Vabysmo®) are also available.
-
What to Expect: Treatment begins with a loading phase of several monthly injections, followed by a maintenance phase where the interval between injections is personalized to your response. This ongoing therapy can dramatically reduce swelling, stabilize vision, and often improve sight.
2. Laser Surgery
Laser remains a highly effective tool, used in two primary ways:
-
Focal/Grid Laser: Used for certain patterns of Diabetic Macular Edema (DME), this laser seals specific leaky vessels to reduce swelling.
-
Panretinal Photocoagulation (PRP or Scatter Laser): This is the benchmark treatment for Proliferative Diabetic Retinopathy (PDR). Hundreds of tiny laser spots are placed in the peripheral retina to reduce its oxygen demand, causing abnormal blood vessels to regress and preventing bleeding or detachment.
3. Corticosteroid Treatments
If anti-VEGF response is insufficient or not an option, corticosteroid injections or long-acting implants may be used to control inflammation and swelling. These are carefully managed by our specialists due to potential side effects, including elevated eye pressure and cataract formation.
4. Vitrectomy Surgery
This microsurgical procedure is necessary for advanced complications. It involves removing the vitreous gel from the middle of the eye to:
-
Clear non-resolving vitreous hemorrhage (blood that won’t clear on its own).
-
Repair a tractional retinal detachment by relieving scar tissue pulling on the retina.
-
Often, laser or other treatments are applied during the same surgery.
How Often Should You Have Follow-Up Exams? A Monitoring Guide
Regular monitoring is your best defense against vision loss from diabetic retinopathy. The frequency of your dilated eye exams at Cannon EyeCare is carefully tailored to your specific condition and overall health. Here’s a general guide based on current standards:
-
No Diabetic Retinopathy: An annual comprehensive dilated eye exam is essential for early detection.
-
Mild to Moderate NPDR: Exams are typically needed every 6 to 12 months to monitor for progression.
-
Severe NPDR or PDR: Requires more vigilant monitoring, often every 2 to 4 months, to determine if and when treatment should begin.
-
Active DME or Receiving Treatment (e.g., injections): Follow-up is most frequent, usually aligned with your treatment cycle (e.g., monthly during initial therapy) to assess response and adjust the plan.
Your schedule will be personalized. Factors that necessitate more frequent monitoring include:
-
Pregnancy
-
Rapid improvement in A1C levels
-
Poorly controlled high blood pressure or cholesterol
-
The presence of kidney disease
Can You Prevent or Slow Diabetic Retinopathy? Yes, Here’s How.
While a diabetes diagnosis comes with risks, vision loss from diabetic retinopathy is largely preventable. Proactive management is the key to protecting your sight. Here are the most effective, practical steps you can take:
1. Master Your Blood Sugar Control
This is the single most important factor. Reaching and maintaining your target A1C level significantly reduces your risk of developing DR and dramatically slows its progression if it has already started. Consistent blood sugar management is your foundation.
2. Manage Your Overall Health
Your eyes are connected to your whole body. Comprehensive care is essential:
-
Control Blood Pressure: High pressure damages delicate retinal vessels.
-
Manage Cholesterol: Healthy lipid levels support better vascular health.
-
Quit Smoking: Tobacco use significantly accelerates vascular damage.
This means coordinated care between your primary care doctor, your endocrinologist, and your eye specialist is crucial for your long-term outcomes.
3. Commit to Annual Dilated Eye Exams
Do not wait for symptoms. Annual comprehensive dilated eye exams at Cannon EyeCare are non-negotiable. They allow for early detection and timely intervention, which is one of the most effective ways to protect your sight. If you have been diagnosed with any stage of DR, you will need more frequent monitoring as directed by our doctors.
Diabetic retinopathy is a common, preventable cause of vision loss in people with diabetes, and early detection plus risk‑factor control dramatically improve outcomes over the long term. Annual eye exams, modern imaging, and targeted therapies like anti‑VEGF injections and PRP help prevent progression and preserve sight when applied early and monitored regularly. National data demonstrate a large burden, and local practices like Cannon EyeCare focus on accessible, guideline‑based care to reduce vision loss across Seattle’s communities.
Schedule your comprehensive diabetic eye exam today at Cannon EyeCare to protect your vision for life.
FAQs
-
It’s diabetes-related damage to the retina’s tiny blood vessels that can cause leakage, swelling, or abnormal new vessels, leading to vision loss without early treatment