Dry Eye Disease vs Syndrome: What’s the Difference?
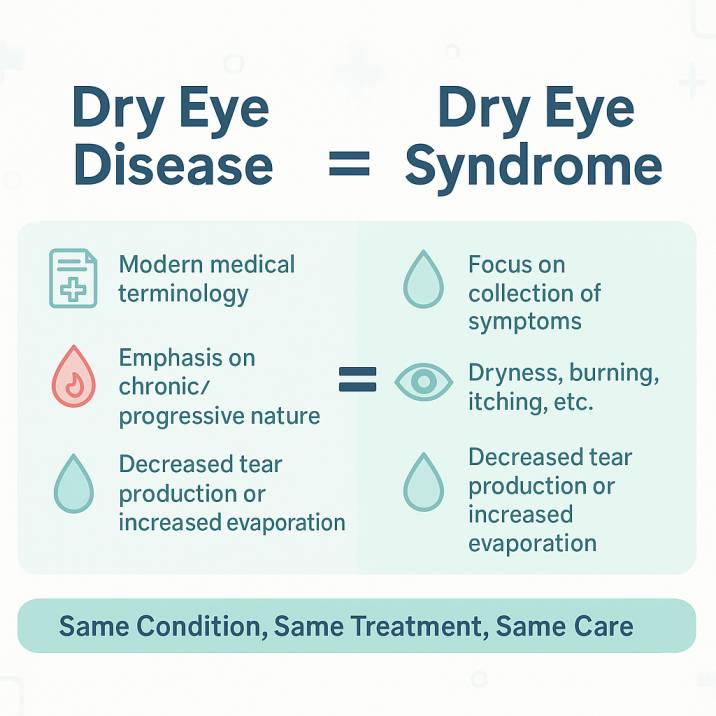
Quick Answer: Dry Eye Disease and Dry Eye Syndrome are the same condition—simply different names used across the medical community. Whether your doctor uses “disease” or “syndrome,” you’re dealing with the same treatable eye condition affecting tear film stability and ocular surface health.
Bottom Line Up Front: Understanding this terminology eliminates confusion, helps you communicate effectively with eye care providers, research treatment options confidently, and ensures you receive appropriate care regardless of which term your doctor prefers.
Understanding the Terminology: Why Two Names for One Condition?
If you’ve researched eye discomfort symptoms, you’ve likely encountered both “Dry Eye Disease” and “Dry Eye Syndrome” and wondered whether you’re facing two distinct conditions. The reassuring truth: you’re not experiencing multiple problems, nor are you misunderstanding your diagnosis.
These terms describe the same multifaceted condition affecting millions worldwide. The terminology variation stems from the natural evolution of medical understanding. As researchers have deepened their knowledge of this condition over the past two decades, different medical practitioners, institutions, and regions have adopted varying terminology preferences.
The Medical Reality
Some eye care professionals prefer “disease” to emphasize the serious, chronic nature of the condition. Others favor “syndrome” to highlight the constellation of symptoms patients experience. Both approaches are medically accurate and appropriate.
Consider this analogy: whether you call a carbonated beverage “soda” or “pop,” you’re discussing the same refreshing drink. Similarly, the medical community simply hasn’t converged on universal terminology—yet both terms describe identical pathophysiology and treatment approaches.
Clinical Significance: Why the Terminology Evolution Matters
From “Syndrome” to “Disease”: A Paradigm Shift
Historically, medical professionals used “Dry Eye Syndrome” when viewing the condition primarily as a collection of symptoms related to insufficient tear production. However, advancing research has revealed the complex interplay of inflammatory, neurological, and anatomical factors involved.
Many specialists now prefer “Dry Eye Disease” because it better reflects the condition’s:
- Chronic, progressive nature requiring ongoing management
- Multifactorial complexity involving inflammation, gland dysfunction, and nerve abnormalities
- Serious health implications affecting vision function and quality of life
- Pathophysiological foundation with measurable biomarkers and objective signs
What This Means for Patients
When you visit an eye care specialist—whether at Cannon EyeCare in University Village, Pike Place Market, or any qualified practice—remain focused on your treatment plan and symptom management rather than terminology differences. Whether your doctor uses “dry eye disease,” “dry eye syndrome,” or the technical term “keratoconjunctivitis sicca,” they’re addressing the same underlying condition.
Understanding Your Condition: The Complete Clinical Picture
Pathophysiology: What Happens
Regardless of terminology, the fundamental problem remains consistent. Healthy vision depends on a stable, three-layered tear film:
- Lipid (oil) layer — Prevents tear evaporation and provides optical smoothness
- Aqueous (water) layer — Delivers moisture, nutrients, and antimicrobial protection
- Mucin layer — Ensures even tear distribution across the eye surface
When any layer becomes compromised, patients experience the symptoms associated with both “dry eye disease” and “dry eye syndrome.”
Classification by Underlying Mechanism
Evaporative Dry Eye (82.5% of cases)
- Primarily caused by Meibomian Gland Dysfunction (MGD), affecting approximately 21.2% of the U.S. population. An insufficient oil layer leads to rapid tear evaporation.n
- Symptoms typically worsen in air-conditioned environments, wind, or low-humidity conditions.
Aqueous Deficient Dry Eye (17.5% of cases)
- Results from inadequate water production by the lacrimal glands
- Often associated with autoimmune conditions such as Sjögren’s syndrome
- May correlate with systemic health conditions or certain medications
Mixed Type
- A combination of both evaporative and aqueous-deficient mechanisms
- Requires comprehensive, multi-modal treatment approaches
Common Symptoms: What to Watch For
Recent 2024-2025 research indicates that approximately 16-20 million Americans are affected by dry eye, with the condition demonstrating significant age-related increases in prevalence. Current estimates suggest around 6.8% of the adult population has diagnosed dry eye, though global prevalence studies indicate the actual number may be as high as 11.6% when including undiagnosed cases.
Primary Symptoms
- Persistent dryness or grittiness
- Burning or stinging sensations
- Feeling like something is “stuck” in your eye
- Blurred or fluctuating vision
- Light sensitivity (photophobia)
- Eye fatigue, especially with screen use
Paradoxical Symptoms
Excessive tearing: This seems counterintuitive, but poor-quality tears often trigger reflex tearing as your eyes attempt to compensate for the underlying problem.
Worse symptoms throughout the day: Many patients notice their discomfort increases as the day progresses, particularly in challenging environments.
Contemporary Treatment Paradigms: Evidence-Based Management Strategies
Foundation Therapies
- Preservative-free artificial tears — Primary treatment for mild symptoms, used 3-4 times daily
- Lid hygiene protocols — Warm compresses and gentle cleaning to optimize meibomian gland function
- Environmental modifications — Humidification, protective eyewear, and strategic screen time management
Prescription Interventions
Anti-inflammatory Medications:
- Cyclosporine (Restasis, Cequa) — Reduces inflammation and stimulates natural tear production; Restasis costs $200-400 monthly, while Cequa offers similar efficacy at reduced cost
- Lifitegrast (Xiidra) — Targets specific inflammatory pathways; retail price exceeds $1,000 monthly without insurance, though discount programs may reduce costs to $600-700
Novel Therapeutic Approaches:
- Varenicline nasal spray (Tyrvaya) — First FDA-approved nasal spray for dry eye, stimulating trigeminal pathways
- Perfluorohexyloctane (Miebo) — Revolutionary 2023 FDA approval specifically targeting tear evaporation
Advanced In-Office Procedures
- Intense Pulsed Light (IPL) therapy — Addresses underlying meibomian gland dysfunction through controlled thermal treatment
- Thermal expression systems — LipiFlow and similar technologies provide mechanical gland clearance
- Punctal occlusion — Strategic tear conservation through temporary or permanent plugs
Emerging Therapeutic Horizons
Current 2024-2025 research developments include:
- Miebo (perfluorohexyloctane) — First prescription specifically targeting evaporative mechanisms
- Lotilaner (Xdemvy) — Addresses Demodex blepharitis-associated dry eye
- Reproxalap — Phase III clinical trials demonstrating promising anti-inflammatory results
- Biologic therapies — Targeted treatments addressing specific inflammatory cascades and nerve growth factors
When to Seek Professional Care
Red Flag Symptoms Requiring Immediate Attention
- Suddenly, severe eye pain
- Significant vision changes
- Symptoms affecting only one eye
- Signs of infection (discharge, severe redness)
- Inability to keep eyes open comfortably
When to Seek Professional Eye Care in Seattle
If you’re experiencing persistent symptoms for more than a few weeks, schedule a comprehensive eye examination with a qualified eye care specialist. In the Seattle area, look for providers who offer:
- Advanced diagnostic technology (tear film analysis, meibomian gland imaging)
- Comprehensive treatment options beyond basic artificial tears
- Experience with both traditional and emerging therapies
- Patient education and personalized care approaches
Ready to find relief from your dry eye symptoms? Contact our experienced team at Cannon EyeCare for a thorough evaluation and personalized treatment plan. With locations in University Village and Pike Place Market, we combine Midwestern hospitality with cutting-edge dry eye care, helping Seattle-area patients achieve comfortable, healthy vision.
Quality of Life Impact: Beyond Physical Discomfort
Functional Implications
Untreated dry eye significantly impacts multiple life domains:
Professional productivity — Difficulty with computer-intensive tasks, prolonged reading, and detail-oriented work
Mental health — Increased rates of depression and anxiety among patients with chronic symptoms
Social engagement — Avoidance of environments that exacerbate symptoms (air-conditioned spaces, outdoor activities)
Sleep quality — Nocturnal symptoms disrupting rest and recovery
Economic Burden
Clinical research demonstrates that severe dry eye affects quality of life comparably to moderate-to-severe angina. The U.S. dry eye treatment market reached $2.45 billion in 2024, with projected growth at 6.0% annually through 2030, underscoring the substantial healthcare investment required for effective management.
This economic reality emphasizes why proper diagnosis and evidence-based treatment represent essential investments in long-term well-being and functional capacity.
Patient Communication: Talking with Your Eye Care Provider
Questions to Ask During Your Appointment
- “What type of dry eye do I have – evaporative, aqueous deficient, or mixed?”
- “What underlying factors might be contributing to my condition?”
- “How will we measure treatment success?”
- “What lifestyle modifications should I prioritize?”
- “When should I expect to see improvement?”
Information to Share
- Complete symptom timeline
- Current medications (including over-the-counter)
- Work environment details
- Screen time habits
- Previous treatments attempted
Future Directions in Dry Eye Management
Personalized Medicine Initiatives
The field is advancing toward individualized treatment protocols based on:
Genetic profiling — Understanding inherited predispositions to inflammatory responses
Biomarker analysis — Targeting specific inflammatory pathways identified through tear film analysis
Environmental assessment — Customizing care protocols for individual lifestyle and occupational factors
Advanced diagnostics — Utilizing artificial intelligence for precise phenotyping and treatment selection
Emerging Research Frontiers
- Regenerative therapeutics — Stem cell applications for severe, refractory cases
- Gene therapy approaches — Addressing genetic components of tear film dysfunction.n
- Ocular microbiome research — Understanding bacterial ecosystem influences on surface health
- Nanotechnology applications — Enhanced drug delivery systems for improved therapeutic outcomes
Evidence-Based Self-Management Strategies
Environmental Optimization
- Humidity control — Maintain indoor humidity levels between 40-60% using quality humidification systems
- Digital ergonomics — Position computer monitors below eye level to reduce lid aperture and evaporation
- Visual hygiene — Implement the 20-20-20 rule: every 20 minutes, focus on objects 20 feet away for 20 seconds
- Protective eyewear — Utilize wraparound sunglasses during outdoor activities to minimize environmental exposure
Nutritional Support Strategies
- Omega-3 fatty acids — Clinical evidence supports 2000mg daily supplementation for anti-inflammatory benefits
- Systemic hydration — Maintain adequate fluid intake to support overall tear production capacity
- Anti-inflammatory nutrition — Emphasize foods rich in antioxidants and minimize pro-inflammatory dietary components
Technology Integration
- Blue light filtration — May provide symptomatic relief during extended screen use
- Environmental monitoring — Air quality assessment to identify and minimize exposure to irritants
- Symptom tracking applications — Digital monitoring of symptoms, triggers, and treatment responses for optimal management
Clinical Conclusions: Evidence-Based Recommendations
Essential Understanding:
- Terminology uniformity — “Dry eye disease” and “dry eye syndrome” describe identical pathophysiological processes requiring consistent treatment approaches
- Early intervention imperative — Prompt professional evaluation prevents progression to more severe, refractory presentations
- Individualized management — Treatment success requires personalized protocols addressing specific underlying mechanisms
- Realistic expectations — Most therapeutic interventions require 4-6 weeks for clinical efficacy, with some treatments necessitating 2-3 months for optimal results
- Chronic condition management — Long-term success depends on consistent care and regular monitoring rather than isolated interventions
Clinical Action Steps
For patients experiencing persistent ocular discomfort, schedule a comprehensive evaluation with an eye care specialist experienced in ocular surface disease management. Remember that effective treatment transcends terminology—whether your provider uses “dry eye disease” or “dry eye syndrome,” you’re receiving care for a well-characterized condition with numerous evidence-based treatment options.
Professional care coordination ensures appropriate diagnosis, individualized treatment planning, and ongoing monitoring for optimal long-term outcomes. The terminology confusion that initially brought you to this information shouldn’t distract from the most crucial fact: effective, scientifically-validated treatments are available, and most patients achieve significant symptomatic improvement through comprehensive, professionally-guided management.
Ready to find relief from your dry eye symptoms? Contact our experienced team at Cannon EyeCare for a thorough evaluation and personalized treatment plan. We understand the latest advances in dry eye care and are committed to helping you achieve comfortable, healthy vision.
Key Resources and Citations
1. Tear Film and Ocular Surface Society (TFOS) – Official Definition
Source: TFOS DEWS II Report – Epidemiology Report
Link: https://www.tfosdewsreport.org/report-epidemiology_report/71_36/en/
Citation: TFOS DEWS II defines dry eye as “a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiologic roles.”
Why This Matters: This is the gold standard definition used worldwide by eye care professionals and researchers, providing the authoritative medical foundation for understanding both “dry eye disease” and “dry eye syndrome” as the same condition.
2. Recent Prevalence and Market Analysis
Source: U.S. Dry Eye Syndrome Treatment Market Size Report, 2030
Link: https://www.grandviewresearch.com/industry-analysis/us-dry-eye-syndrome-treatment-market-report
Citation: The U.S. dry eye syndrome treatment market size was estimated at USD 2.45 billion in 2024 and is projected to grow at a CAGR of 6.0% from 2025 to 2030. Market growth in the country is driven by the high prevalence of dry eye disease (DED), which affects approximately 20 million Americans.
Why This Matters: This provides current 2024 statistics on prevalence and economic impact, demonstrating the significant scope of the condition regardless of terminology used, and supporting the article’s emphasis on why proper understanding matters.
3. Medical Literature on Terminology Clarity
Source: StatPearls – Dry Eye Syndrome (National Library of Medicine)
Link: https://www.ncbi.nlm.nih.gov/books/NBK470411/
Citation: Dry eyes, also known as dry eye syndrome (DES), dry eye disease (DED), ocular surface disease (OSD), dysfunctional tear syndrome (DTS), and keratoconjunctivitis sicca (KCS), are among the most common reasons for a visit to an eye doctor. Even though the names are frequently used interchangeably, it can be confusing because different medical practitioners and researchers use different terminologies.
Why This Matters: This authoritative medical resource directly addresses the terminology confusion that patients experience, validating the article’s main premise that both terms describe the same condition while acknowledging the legitimate confusion this creates.
Additional Supporting Research:
- Frontiers in Medicine 2024 study on the quality of life impact
- Scientific Reports 2024 prevalence study among medical students
- American Journal of Ophthalmology 2019 large-scale U.S. population study
- Multiple 2024 market research reports confirming treatment advances and costs
These sources provide the medical authority, current statistics, and patient-focused perspective that form the foundation of this comprehensive guide to understanding dry eye terminology and treatment options.
FAQs
-
There’s no difference; both terms describe the same condition where your eyes don’t produce enough quality tears or tears evaporate too quickly