Dry Eye in Seattle: Causes, Symptoms & Relief
Executive Summary & Key Takeaways
Seattle residents face unique challenges with dry eye symptoms due to the region’s distinctive climate patterns—from windy conditions that accelerate tear evaporation to seasonal indoor heating that creates dry environments. Understanding your symptoms and seeking proper professional evaluation can prevent complications and restore comfort through personalized treatment approaches that range from simple lifestyle modifications to advanced in-office therapies.
Understanding Dry Eye Symptoms
Dry eye disease affects millions of Americans, with recent studies indicating that an estimated 5% to 50% of the global population experiences dry eye symptoms, with women and older adults being more susceptible. For Seattle residents, this common condition can significantly impact daily activities from reading and computer work to driving, especially when compounded by the region’s environmental factors.
Bottom Line: Dry eye is a chronic, progressive condition that requires ongoing management rather than a one-time cure, similar to conditions like high blood pressure or diabetes.
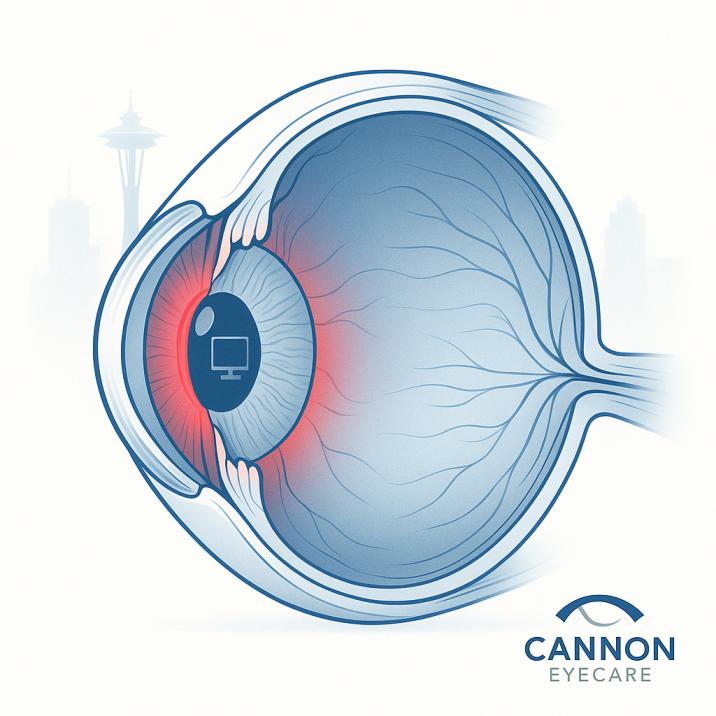
The Science Behind Dry Eye
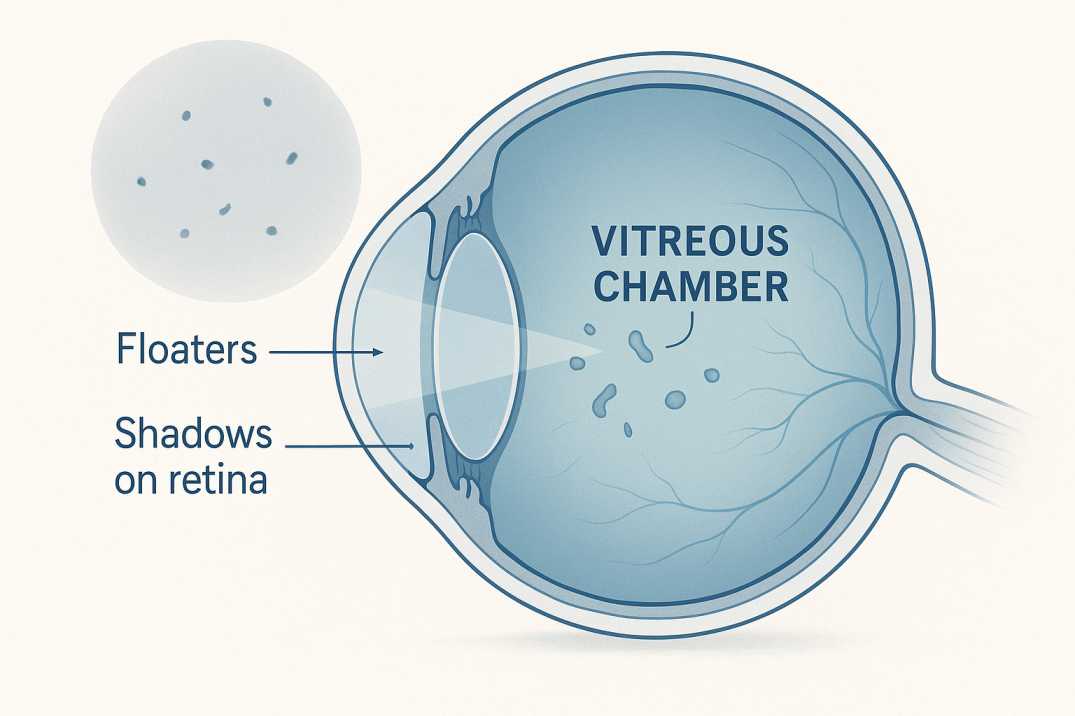
Dry eye disease occurs when your tear film—the protective layer covering your eye’s surface—becomes unstable or insufficient. According to the Tear Film and Ocular Surface Society (TFOS) Dry Eye Workshop II (DEWS II), dry eye is “a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation” create a cascade of problems.
Your tear film consists of three essential layers:
- Lipid (oil) layer: Produced by meibomian glands to prevent evaporation
- Aqueous (water) layer: Created by lacrimal glands for lubrication
- Mucin layer: Made by conjunctival cells to help tears adhere to the eye surface
When any of these layers becomes disrupted, dry eye symptoms develop.
Seattle’s Climate and Dry Eye Triggers
Seattle’s unique Pacific Northwest climate creates specific challenges for dry eye sufferers. The region’s combination of seasonal weather patterns, indoor heating systems, and urban environmental factors can exacerbate symptoms throughout the year.
Seasonal Impacts on Dry Eye
Winter Months: Symptoms tend to be worse on windy days and during the winter months due to dry indoor heat. Seattle’s heating systems reduce indoor humidity, while cold outdoor air holds less moisture, creating a double challenge for tear film stability.
Spring and Fall: Variable weather patterns with frequent wind can accelerate tear evaporation. Seattle’s average wind speeds during transitional seasons can particularly affect those with compromised tear production.
Summer: While generally milder, air conditioning usage and outdoor activities in sunny conditions can contribute to increased tear evaporation.
Urban Environmental Factors
Seattle’s urban environment presents additional challenges:
- Air pollution from traffic and industry
- Digital eye strain from the tech-heavy workforce
- Reduced blinking rates during screen-intensive work
- Indoor air quality is affected by building ventilation systems
Common Causes of Dry Eye Disease
Understanding the underlying causes of dry eye helps Seattle residents identify personal risk factors and make informed treatment decisions.
Primary Causes
Evaporative Dry Eye: Most people who experience dry eye symptoms have what is known as evaporative dry eye. Evaporative dry eye occurs when the tear film coating the eye evaporates too quickly because of insufficient oil (lipid) content. This is most often the result of a blockage in the Meibomian glands.
Aqueous Deficient Dry Eye: Occurs when tear glands produce insufficient quantities of tears, often related to:
- Age-related decrease in tear production
- Autoimmune conditions like Sjögren’s syndrome
- Hormonal changes, particularly in women
- Certain medications
Contributing Factors Specific to Seattle Residents
Demographics: Seattle’s aging population faces increased risk, as tear production tends to diminish as you get older. Dry eyes are more common in people over 50.
Gender: A lack of tears is more common in women, especially if they experience hormonal changes due to pregnancy, using birth control pills, or menopause.
Lifestyle Factors:
- Extended computer use in tech industry jobs
- Contact lens wear
- Air conditioning and heating exposure
- Dietary factors, including insufficient omega-3 fatty acids
Medical Conditions: Certain medical conditions, including Sjogren’s syndrome, allergic eye disease, rheumatoid arthritis, lupus, scleroderma, graft vs. host disease, sarcoidosis, thyroid disorders, or vitamin A deficiency.
Medications: Certain medicines, including antihistamines, decongestants, hormone replacement therapy, antidepressants, and medicines for high blood pressure, acne, birth control, and Parkinson’s disease.
Recognizing Dry Eye Symptoms
Dry eye symptoms can vary significantly between individuals and may not always be obvious initially. Understanding the full spectrum of symptoms helps Seattle residents identify when professional evaluation is needed.
Primary Dry Eye Symptoms
Classic Symptoms:
- Burning, irritation, and itching, as well as tearing or watering eyes
- Dryness – a constant sandy or scratchy sensation
- Eye pain or discomfort
- Blurred vision. One clue that blurred vision is due to dry eye is that it clears temporarily after blinking.
Paradoxical Symptoms: Watery eyes (counterintuitive, but a hallmark symptom) occur because the surface of the eye is dry and sends a signal to the brain to secrete more tears and moisturize the cornea. However, the mostly reflex tears that are secreted by the lacrimal and accessory lacrimal (tear) glands may be of poor quality.
Activity-Related Symptoms
Dry eye symptoms can be especially troublesome while reading, watching TV, and working on the computer—activities that are particularly relevant for Seattle’s professional workforce.
Environmental Trigger Dry Eye Symptoms
Symptoms often worsen with:
- Wind exposure (common in Seattle)
- Air conditioning or heating
- Smoke or air pollution
- Low-humidity environments
Progressive Nature of Symptoms
Dry eye is a chronic and progressive condition that affects quality of life by its host of ocular symptoms and its ability to impact patient productivity at work and home. Early recognition and treatment can prevent progression to more severe stages.
Professional Diagnosis and Evaluation
Accurate diagnosis requires professional evaluation, as dry eye symptoms can mimic other conditions, and self-diagnosis may lead to inappropriate treatment choices.
Comprehensive Dry Eye Assessment
Professional evaluation typically includes:
Medical History Review: We will inquire about the patient’s symptoms, such as dryness, irritation, redness, fluctuating vision, and sensitivity to light. Providing detailed information about the frequency and severity of symptoms can aid in the diagnosis.
Tear Film Analysis: The quality and quantity of the tear film are assessed through various tests, such as tear breakup time (TBUT), Schirmer’s test, and tear osmolarity measurement. These tests help determine the stability and production of tears.
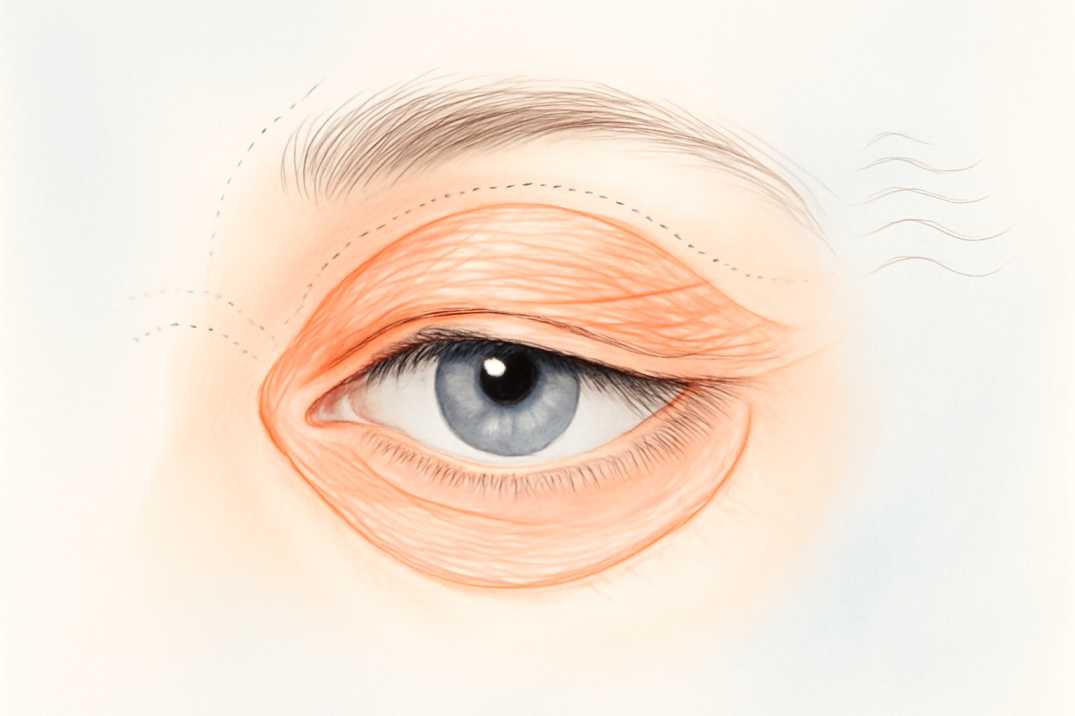
Ocular Surface Examination: To diagnose dry eye, the doctor will look closely at your eyelids, check the quality of your tear film, and check for ocular inflammation.
Advanced Diagnostic Technology
Seattle eye care providers often utilize state-of-the-art diagnostic equipment:
- Tear film osmolarity testing
- Meibography to assess oil gland function
- Inflammatory marker testing
- Digital imaging of tear breakup patterns
Identifying Root Causes
A dry eye evaluation at Cannon EyeCare identifies root causes (e.g., tear quality or environmental factors) to create a tailored management plan. This personalized approach is crucial for effective long-term management.
Treatment Options for Seattle Residents
Treatment approaches have expanded significantly in recent years, offering Seattle residents multiple options ranging from conservative home care to advanced in-office procedures.
Conservative Management
Artificial Tears: In general, artificial tears remain a mainstay of treatment for dry eye symptoms. Many brands of artificial tears are available, and they vary in their composition, active ingredients, preservatives, etc. Patients with severe dry eyes are usually prescribed preservative-free artificial tears.
Home Care Treatments: Many cases of dry eye can be treated with home care steps, including eyelid cleaning products, dry eye masks, and artificial tears.
Warm Compress Therapy: Heat will soften the oils, allowing for easier release from the meibomian glands. Studies have proven that meibomian secretions melt at 32 – 45°C (89.6 – 113°F). It takes about 10 minutes for heat to fully penetrate the tarsal plates and reach 40°C at the inner eyelid.
Prescription Medications
Anti-inflammatory Treatments: When artificial tears do not reduce the symptoms of dry eyes, other medications such as topical cyclosporin (Restasis) or topical steroids may be prescribed. Topical cyclosporin is used twice daily and takes 6-12 weeks to have an effect.
Tear Stimulating Medications: Tear-stimulating eye drops that are prescribed to help increase your body’s natural tear production. Anti-inflammatory eye drops are used to reduce inflammation on the corneal and ocular surface.
Advanced In-Office Treatments
Intense Pulsed Light (IPL): Intense Pulsed Light (IPL) Therapy addresses the underlying inflammation associated with dry eye by unclogging the meibomian glands and encouraging healthy tear production.
Meibomian Gland Expression: Meibomian gland expression is a procedure that clears blocked oil glands, which prevents the rapid evaporation of tears.
LipiFlow Treatment: Lipiflow applies a gentle warm heat to the internal eyelids along with a thermal pulsation to gently and safely massage your eyelids. This combination of warmth and massage helps to unclog the glands that limit the quality of oil in the tears.
Punctal Plugs: Small devices inserted into the tear ducts, called punctal plugs, can block tear drainage, helping to keep the eye surface moist for longer.
Emerging Therapies
Recent advances include:
- Amniotic Extract Eye Drops: Containing nutrients and anti-inflammatory properties, amniotic extract eye drops have proven to help alleviate advanced dry eye symptoms in many people
- Radio Frequency Treatment: Radio Frequency (RF) Treatment – This stimulates your body into rejuvenating the oil glands back to working order. Results help your body to help itself maintain tearfilm and hydration on your eyeballs.
Treatment Success Rates
In most cases, we can significantly improve the symptoms of dry eye with adequate hydration, working on eyelid health, and the use of artificial tears or medicated drops. Our optometrists would rarely refer for surgical intervention.
Prevention Strategies
Preventing dry eye or minimizing symptom progression involves addressing modifiable risk factors and implementing protective lifestyle habits.
Environmental Modifications
Indoor Air Quality:
- Use humidifiers during heating season (especially important in Seattle winters)
- Position fans and air vents away from direct eye exposure
- Add moisture to the air. In winter, a humidifier can add moisture to dry indoor air.
Eye Protection:
- Consider wearing wraparound sunglasses or other protective eyewear. Safety shields can be added to the tops and sides of eyeglasses to block wind and dry air.r
- Use computer glasses with the anti-reflective coating
Digital Eye Strain Prevention
The 20-20-20 Rule: Take eye breaks during long tasks. If you’re reading or doing another task that requires visual concentration, take periodic eye breaks. Close your eyes for a few minutes. Or blink repeatedly for a few seconds to help spread your tears evenly over your eyes.
Workspace Optimization:
- Position screens at or slightly below eye level
- Maintain an arm’s length distance from screens
- Ensure adequate lighting to reduce glare
- Use artificial tears during extended computer sessions
Lifestyle Modifications
Dietary Considerations: Eating a diet that is low in vitamin A, which is found in liver, carrots, and broccoli, or low in omega-3 fatty acids, which are found in fish, walnuts, and vegetable oil, can contribute to dry eye symptoms.
Hydration: Maintaining adequate systemic hydration supports tear production.
Sleep Quality: Proper sleep hygiene supports overall eye health and tear production.
When to Seek Professional Care
Understanding when symptoms require professional attention can prevent complications and improve treatment outcomes.
Red Flag Symptoms
Seek immediate professional evaluation for:
- Sudden onset of severe dry eye symptoms
- Eye pain that doesn’t improve with artificial tears
- Significant vision changes
- Signs of infection (discharge, severe redness)
- Symptoms affecting daily activities or work productivity
Early Intervention Benefits
See your health care provider if you’ve had prolonged signs and symptoms of dry eyes, including red, irritated, tired, or painful eyes. Your provider can take steps to determine what’s bothering your eyes or refer you to a specialist.
Potential Complications
Yes—chronic dry eye can lead to corneal scarring or infections if untreated. Early evaluation at Cannon EyeCare Seattle helps prevent complications through timely, targeted therapies.
People who have dry eyes may experience these complications: Eye infections. Your tears protect the surface of your eyes from infection. Without adequate tears, you may have an increased risk of eye infection. Damage to the surface of your eyes. If left untreated, severe dry eyes may lead to eye inflammation, abrasion of the corneal surface, corneal ulcers, and vision loss.
Recent Scientific Advances
The field of dry eye research continues to evolve rapidly, with new understanding of disease mechanisms and treatment approaches emerging regularly.
Market Growth and Research Investment
The global Dry Eye Syndrome market is projected to reach USD 7,940 million by 2032, expanding at a CAGR of 5.9% from 2025 to 2032, reflecting significant investment in research and development.
New Treatment Approaches
Recent research has identified new biologics, stem cell therapy, gene therapy, and nanotechnology for drug delivery, offering new hope and directions for DED treatment, laying a foundation for future research.
Understanding of Disease Mechanisms
Recent research indicates that approximately 11.59% of the global population is affected by dry eye disease, with global prevalence varying by region and diagnostic criteria. For symptomatic disease, prevalence is estimated at 9.12%, with women (9.5%) more affected than men (6.8%).
Three Recent Scientific Studies
-
Immunotherapy Research (2024): A comprehensive review published in Frontiers in Ophthalmology examined multidimensional immunotherapy for dry eye disease, focusing on immune dysregulation and neuro-immune interactions. This research provides new insights into why traditional treatments sometimes fail and points toward more targeted therapeutic approaches.
-
Pediatric Dry Eye Study (2025): A systematic review and meta-analysis published in BMJ Open Ophthalmology found that the prevalence of DED was 18.7% before and 44.1% after the COVID-19 outbreak among children, highlighting the impact of increased screen time and environmental changes on younger populations.
-
Quality of Life Impact Research (2024): A study published in Frontiers in Medicine examined the impact of dry eye disease treatment on patient quality of life, providing evidence-based support for comprehensive treatment approaches that address both objective signs and subjective symptoms.
Clinical Application of New Research
The future of dry eye management is characterized by precision, technological integration, and a deeper understanding of the multifactorial nature of the condition. An ongoing commitment to research and development will ensure that we continue to meet the evolving needs of our patients.
Resources and Citations
This article is based on peer-reviewed research and authoritative medical sources to ensure accuracy and reliability. Below are key resources used:
1. Tear Film and Ocular Surface Society (TFOS) DEWS II Report
Source: Craig, J.P., Nelson, J.D., Azar, D.T., et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(4):802-812.
Link: https://www.sciencedirect.com/science/article/pii/S1542012417300486
Usage: Primary definition of dry eye disease, classification systems, and diagnostic criteria used throughout the article.
2. Global Prevalence Research – Bayesian Meta-Analysis
Source: Clayton, J.A. The global prevalence of dry eye disease: A Bayesian view. PubMed. 2021.
Link: https://pubmed.ncbi.nlm.nih.gov/34545606/
Usage: Current global prevalence statistics (11.59% overall prevalence, 9.12% symptomatic disease) and demographic breakdowns by gender.
3. Meibomian Gland Temperature Research
Source: Borchman, D., et al. The optimum temperature for the heat therapy for meibomian gland dysfunction. Exp Eye Res. 2019;180:162-169.
Link: https://www.sciencedirect.com/science/article/abs/pii/S154201241830404X
Usage: Scientific data on meibomian secretion melting points (30-32°C) and optimal therapeutic temperatures (40°C+) for warm compress therapy.
Additional Medical Resources
- Mayo Clinic Dry Eye Disease Information: Comprehensive patient education materials on symptoms and risk factors
- American Academy of Ophthalmology: Professional guidelines for dry eye diagnosis and treatment
- National Eye Institute: Population health data and research funding information
Clinical Summary and Practice Implications
Dry eye disease represents a complex, multifactorial condition requiring nuanced diagnostic evaluation and individualized therapeutic approaches. For Pacific Northwest practitioners, understanding regional environmental factors enhances clinical assessment and treatment planning effectiveness.
Seattle’s distinctive meteorological patterns—characterized by seasonal humidity variations, prevalent wind exposure, and extensive indoor climate control—create specific challenges for ocular surface health maintenance. Healthcare providers must incorporate these environmental considerations when developing management strategies for local patient populations.
Key Clinical Takeaways
Contemporary evidence supports several critical practice points:
- Early intervention significance: Timely professional evaluation prevents disease progression and reduces the risk of irreversible ocular surface damage, including corneal scarring and infectious complications
- Environmental modification importance: Strategic lifestyle adjustments addressing Seattle’s specific climate challenges often provide substantial symptomatic improvement.
- Treatment individualization necessity: Therapeutic success requires personalized approaches accounting for disease subtype, severity, and patient-specific risk factors
- Multidisciplinary care value: Optimal outcomes emerge through coordinated management addressing both underlying pathophysiology and symptomatic manifestations
Future Practice Directions
The evolution toward precision medicine in dry eye management promises enhanced therapeutic outcomes through biomarker-guided treatment selection and personalized intervention protocols. Continued research investment in regenerative therapies, novel drug delivery systems, and environmental mitigation strategies offers hope for improved patient quality of life.
Healthcare practitioners serving the Seattle metropolitan area are uniquely positioned to advance dry eye care through integration of evidence-based medicine with region-specific environmental expertise. This comprehensive approach enables optimal patient outcomes while contributing to the broader understanding of environmental influences on ocular surface disease.
Clinical Action Point: Establish comprehensive dry eye evaluation protocols that incorporate environmental assessment, standardized symptom questionnaires, and objective diagnostic testing to ensure optimal patient care delivery in the Pacific Northwest healthcare setting.
FAQs
-
Dry eyes are caused by low tear production or fast tear evaporation. Risk is higher for adults over 40, screen users, contact lens wearers, and people with allergies or autoimmune conditions