Retinitis Pigmentosa: Causes, Symptoms & Care
Executive Summary: Retinitis pigmentosa affects 1.5-2 million people worldwide, with a prevalence of 1 in 3,000 to 1 in 5,000 individuals. This inherited condition causes progressive vision loss beginning with night blindness and peripheral vision deterioration. Although no cure exists for most forms, emerging gene therapies, assistive technologies, and comprehensive management strategies offer significant potential to preserve remaining vision and maintain independence. Early diagnosis and proactive care planning remain essential for optimal outcomes.
Understanding Retinitis Pigmentosa: Essential Medical Knowledge
Retinitis pigmentosa (RP) represents a group of rare, inherited eye diseases affecting the retina—the light-sensitive tissue layer at the posterior aspect of the eye. This condition causes a gradual breakdown of retinal cells, resulting in progressive vision loss. Despite the term “retinitis” suggesting inflammatory processes, current medical understanding recognizes that inflammation plays a minimal role in disease progression. The condition is more accurately characterized as a retinal dystrophy, indicating gradual degeneration of retinal cellular structures.
This inherited condition constitutes the most prevalent hereditary retinal disease, affecting approximately 1 in every 3,000 to 1 in 5,000 individuals worldwide. The condition typically presents bilaterally, though disease progression patterns may vary between eyes.
Pathophysiology and Vision Impact
Retinal Architecture and Function
The retina contains two primary types of photoreceptor cells: rods and cones. Rod photoreceptors, predominantly located in the peripheral retina, facilitate vision in low-light conditions and provide peripheral visual field coverage. Most forms of retinitis pigmentosa initially affect rod photoreceptors, which explains the characteristic early presentation of nyctalopia (night blindness) and peripheral visual field deficits.
As the disease progresses, cone photoreceptors—concentrated in the central retina and responsible for color vision and visual acuity—also become compromised. This progression pattern results in the characteristic clinical presentation of retinitis pigmentosa.
Clinical Progression and Symptom Development
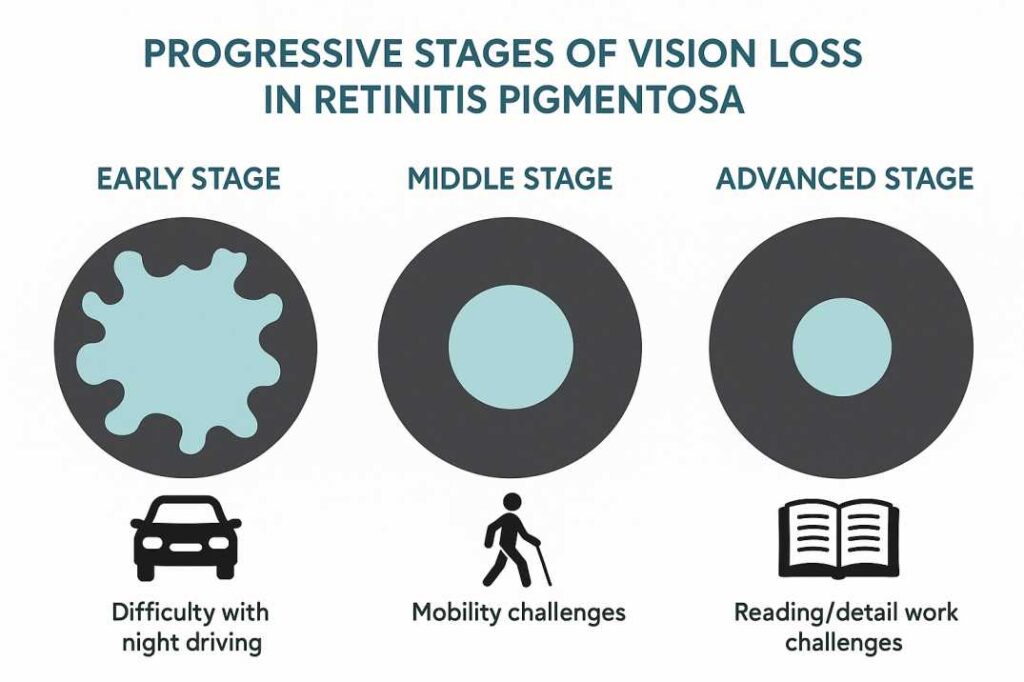
The visual impairment pattern in retinitis pigmentosa follows a predictable sequence:
Initial Stage:
- Nyctalopia (night blindness)—impaired dark adaptation and reduced scotopic vision
- Delayed adjustment when transitioning between varying light conditions
- Caregivers may observe pediatric patients experiencing difficulty navigating in reduced illumination
Intermediate Stage:
- Progressive peripheral visual field constriction—development of ring scotomas
- Gradual evolution toward tunnel vision with preserved central visual acuity
- Compromised mobility and spatial navigation abilities
- Photophobia and increased sensitivity to glare
Advanced Stage:
- Severe concentric visual field restriction with minimal remaining central vision
- Potential involvement of central retinal function
- Compromised color discrimination
- Substantial functional visual impairment by the fourth decade of life in most patients
Clinical Recognition and Symptom Assessment
Primary Clinical Manifestations
Retinitis pigmentosa symptoms include reduced visual function in low-light conditions, diminished peripheral visual field awareness, progressive constriction of functional visual area, and compromised spatial navigation abilities.
Pediatric and Adolescent Presentations:
- Impaired navigation in dimly illuminated environments
- Reduced performance during twilight activities
- Compromised peripheral awareness resulting in contact with obstacles
- Decreased athletic performance in activities requiring peripheral vision
- Prolonged adaptation periods when transitioning between lighting conditions
Adult Progression Indicators:
- Inability to operate vehicles safely during nighttime hours
- Difficulty locating objects in reduced illumination
- Compromised reading ability in suboptimal lighting conditions
- Reduced facial recognition at a distance
Molecular Genetics and Inheritance Patterns
Genetic Architecture and Pathophysiology
Retinitis pigmentosa results from pathogenic variants (mutations) affecting genes essential for retinal function and photoreceptor maintenance. Current research has identified over 100 genes associated with RP, each encoding proteins critical for various aspects of retinal cellular function, including phototransduction cascades, retinoid cycling, photoreceptor structural integrity, and cellular survival mechanisms. This extensive genetic heterogeneity explains the considerable phenotypic variability observed among patients and necessitates individualized therapeutic approaches.
Modes of Inheritance
Retinitis pigmentosa demonstrates multiple inheritance patterns:
Autosomal Dominant Inheritance: A single pathogenic allele is sufficient to cause disease manifestation, typically presenting with milder phenotypes and later onset.
Autosomal Recessive Inheritance: Disease occurs only when both parental alleles carry pathogenic mutations. Parents are typically asymptomatic carriers, with each offspring having a 25% risk of inheriting the condition.
X-linked Inheritance: Pathogenic variants on the X chromosome primarily affect males, while female carriers may exhibit variable phenotypic expression ranging from asymptomatic to severely affected.
Simplex Cases: Approximately 50% of cases occur without identifiable family history, potentially resulting from de novo mutations or incomplete penetrance patterns.
Diagnostic Evaluation and Clinical Assessment
Comprehensive Ophthalmologic Examination
Clinical diagnosis of retinitis pigmentosa requires a comprehensive ophthalmologic evaluation, including dilated funduscopy. This examination involves mydriatic administration to facilitate posterior segment visualization and assessment for characteristic retinal changes associated with RP, including bone spicule pigmentation, arteriolar attenuation, and optic disc pallor.
The diagnostic process requires specialized expertise in inherited retinal diseases to ensure accurate assessment and appropriate referrals. Eye care professionals like those at Cannon EyeCare employ advanced diagnostic protocols specifically designed for complex retinal conditions, ensuring comprehensive evaluation of all relevant clinical parameters.
Advanced Diagnostic Modalities
Electroretinography (ERG): This electrophysiologic test measures retinal cellular electrical responses to light stimulation, providing an objective assessment of photoreceptor function. ERG can detect retinal dysfunction before clinical symptoms become apparent and serves as the gold standard for RP diagnosis.
Kinetic and Static Perimetry: Visual field testing maps peripheral vision boundaries and quantifies functional visual field preservation, essential for disease monitoring and progression assessment.
Optical Coherence Tomography (OCT): High-resolution cross-sectional retinal imaging allows detailed visualization of retinal architecture, including photoreceptor layer integrity and retinal thickness measurements.
Fundus Autofluorescence (FAF) Imaging: This non-invasive imaging modality utilizes retinal lipofuscin autofluorescence to assess retinal pigment epithelium health and photoreceptor viability.
Molecular Genetic Testing: Genetic analysis provides a definitive diagnosis, inheritance pattern determination, and facilitates personalized treatment recommendations. Testing may involve single-gene analysis, multi-gene panels, or comprehensive genomic sequencing.
Therapeutic Interventions and Management Strategies
FDA-Approved Gene Therapy
Voretigene neparvovec-rzyl (Luxturna) represents the first FDA-approved gene therapy for inherited retinal dystrophies, specifically targeting patients with confirmed biallelic RPE65 mutations. This adeno-associated virus vector-based therapy delivers functional RPE65 gene copies via subretinal injection, with treatment costs approximating $850,000 for bilateral administration. Clinical efficacy has been demonstrated in approximately 1,000-2,000 patients in the United States with confirmed biallelic RPE65 mutations who retain viable retinal tissue.
Emerging Therapeutic Modalities
MCO-010 Optogenetic Therapy: This mutation-agnostic gene therapy has demonstrated vision restoration capabilities in patients with advanced retinitis pigmentosa, with clinical trials showing up to 50% of patients achieving significant visual acuity improvements. Unlike Luxturna’s mutation-specific approach, MCO-010 targets multiple genetic variants through optogenetic protein delivery.
N-acetylcysteine (NAC) Clinical Investigation: The NAC Attack Phase III multicenter trial, conducted by Johns Hopkins University, is evaluating oral antioxidant therapy effectiveness across 438 patients at 30 international sites over 45 months.
Autologous Stem Cell Therapy: UC Davis researchers have demonstrated the safety and potential efficacy of CD34+ stem cell therapy through intravitreal administration, with preliminary results showing measurable vision improvements in four of seven treated patients.
Novel Research Approaches
Optogenetic Interventions: Kiora Pharmaceuticals’ KIO-301 photoswitch therapy aims to restore light sensitivity to surviving retinal ganglion cells in patients with advanced disease progression.
Gene-Agnostic Strategies: Nanoscope Therapeutics’ approach utilizes intraocular injection of light-sensitive protein-encoding genes, eliminating the need for external devices while potentially treating multiple genetic variants simultaneously.
Supporting Evidence: Recent Scientific Studies
Study 1: Mutation-Independent Optogenetic Therapy
Researchers with Nanoscope Therapeutics Inc. have announced the publication of a paper, “A synthetic opsin restores vision in patients with severe retinal degeneration,” in Molecular Therapy, the flagship journal of the American Society of Gene & Cell Therapy. This study demonstrated significant vision improvements in patients with advanced RP using optogenetic technology.
Study 2: Stem Cell Safety and Efficacy
“We found the treatment is safe, and four of the seven patients showed measurable improvements in vision” in the UC Davis CD34+ stem cell study. This early-stage trial confirmed both safety and potential therapeutic benefits of autologous stem cell therapy.
Study 3: Gene Therapy Timing Effects
Early and mid treatment restored retinal function to near wild-type levels, specifically the sensitivity and signal fidelity of retinal ganglion cells (RGCs), the ‘output’ neurons of the retina. However, some anatomical defects persisted. Late treatment retinas exhibited continued, albeit slowed, loss of sensitivity. This research emphasizes the importance of early intervention in gene therapy approaches.
Nutritional and Lifestyle Management
Evidence-Based Nutritional Support
Vitamin A may help slow vision loss from the common forms of retinitis pigmentosa. But taking too much vitamin A can cause liver problems — so talk with your doctor about the risks and benefits of this treatment
Recommended Supplements for Inherited Retinal Disease:
- Vitamin A palmitate (under medical supervision)
- Fish oil and lutein supplements may also help slow retinal degeneration
- Avoid excessive vitamin E supplementation
Important Precautions
High levels of vitamin E may worsen retinitis pigmentosa, so people with the condition should avoid taking vitamin E supplementation in excess of 30 IU per day
Light Protection:
- Use UV-filtering sunglasses outdoors
- It is important to protect the retinas from bright sunlight — sunglasses with a UV filter are considered generally protective
Maximizing Vision with Assistive Technologies
Low Vision Aids and Devices for Retinitis Pigmentosa
Vision aids and rehabilitation (training) programs can help people with retinitis pigmentosa make the most of their vision
Magnification Tools:
- Handheld and stand magnifiers
- Electronic reading devices with zoom capabilities
- Some low vision aids and glasses available include telescopic lenses and bioptic systems
Lighting Solutions:
- Using colour contrast to help see things around the home more clearly (e.g., for light switches, buttons, and other everyday items)
- Portable LED lighting for improved visibility
- Anti-glare filters for computer screens
Technology Integration
Smart Device Features:
- Voice-controlled assistants
- Making the most of everyday technology with accessibility features
- GPS navigation apps with audio guidance
Computer Adaptations:
- Screen reading software
- High-contrast display settings
- Keyboard shortcuts and voice recognition
Living Successfully with Retinitis Pigmentosa
Mobility and Independence
At every stage of your experience with RP, there are ways to make the most of your useful vision
Home Modifications:
- Keeping your home tidy and free of obstacles, and keeping regularly used items in a consistent location, so they’re easy to find
- Improved lighting in key areas
- Tactile markers for important controls
Navigation Strategies:
- Orientation and mobility training
- White cane techniques
- Guide dog services when appropriate
Work and Career Considerations
Because RP affects your vision, you’re likely to need some adaptations and adjustments to help you work. Employers are legally required to make reasonable adjustments to support your needs
Workplace Accommodations:
- Adjustable lighting and screen magnification
- Flexible work arrangements
- Accessible transportation options
Transportation and Driving
If you want to drive, you must tell the DVLA that you have retinitis pigmentosa. The law requires drivers to have a minimum field of vision. For individuals with retinitis pigmentosa, driving restrictions often become necessary as peripheral vision deteriorates.
Planning:
- It’s a good idea to plan and find other transport options before you need to stop driving. Look into public transport options near you and alternatives such as taxis.
- Ride-sharing services and community transportation programs
Emotional and Psychological Support
Understanding the Emotional Impact
Three key themes were identified: (1) navigating grief and loss, reflecting the emotional toll of progressive vision loss and the associated loss of independence and cherished activities; (2) establishing independence through coping mechanisms
Common Emotional Responses:
- Grief over vision loss and lifestyle changes
- Anxiety about future progression
- Depression related to activity limitations
- Fear of dependence on others
Building Support Networks
Professional Support:
- Counseling services specialized in vision loss
- Support groups for RP patients and families
- Low vision rehabilitation specialists
Community Resources:
- The support you need to live independently with retinitis pigmentosa is likely to change as the condition gradually affects your sight. However, the earlier you reach out and get support, the easier it can be to adapt to daily life with vision loss.
- Local blindness organizations
- Online communities and forums
Planning for Children and Families
Early Intervention and Education
If your child has been diagnosed with RP, there are a few ways you can support their development both at home and in school
Educational Support:
- It’s a good idea to make your child’s school aware of their condition and how it affects them. Qualified Teachers for Visual Impairment can provide expert support and advice
- Individualized Education Plans (IEPs)
- Assistive technology training
Genetic Counseling: Genetic testing by a certified genetic counselor can help you find out if you are carrying variants in this gene and could be a candidate for gene therapy
Family Planning Considerations
Understanding Inheritance Risks:
- Genetic testing for family members
- Some patients also want to know if their gene variant has a high risk of being passed down to future generations.
- Reproductive counseling options
Research Participation and Clinical Trials
Current Trial Opportunities
At this time, there are no FDA-approved treatments for the other genetic variants that cause retinitis pigmentosa. However, numerous clinical trials are ongoing, some of which address specific genes
Finding Relevant Studies:
- To find current studies on RP, you can search for clinical trials on ClinicalTrials.gov
- Genetic testing to match with appropriate trials
- Research centers specializing in inherited retinal diseases
Contributing to Research Progress
Registry Participation:
- Natural history studies tracking disease progression
- Genetic databases supporting therapy development
- Quality of life research initiatives
Professional Eye Care and Monitoring
Regular Monitoring Importance
People with retinitis pigmentosa need to get regular eye exams. That way, the eye doctor can keep track of symptoms and help find the right treatments
Recommended Follow-up:
- Annual comprehensive eye examinations
- Visual field testing to track progression
- Monitoring for secondary complications
Managing Associated Conditions
People with retinitis pigmentosa can experience other eye conditions that could degrade their vision, such as cataracts and macular edema, or retinal swelling
Treatable Complications:
- Cataract surgery when indicated
- Macular edema management with medications
- Glaucoma monitoring and treatment
Early detection and management of these secondary conditions is crucial for maintaining optimal visual function. Cannon EyeCare’s comprehensive approach includes regular screening for these associated conditions as part of routine retinal care for patients with inherited retinal diseases.
References and Additional Resources
Key Medical and Research Sources
1. National Eye Institute (NEI) – Retinitis Pigmentosa
- URL: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/retinitis-pigmentosa
- Description: Comprehensive resource from the National Institutes of Health providing authoritative information on RP symptoms, diagnosis, and current research developments. Updated regularly with the latest clinical findings and treatment options.
- Key Information Used: Prevalence statistics, diagnostic procedures, vitamin supplementation guidelines, and current research initiatives.
2. Johns Hopkins Medicine – Retinitis Pigmentosa Center
- URL: https://www.hopkinsmedicine.org/health/conditions-and-diseases/retinitis-pigmentosa
- Description: A Leading medical institution’s comprehensive guide covering genetic counseling, clinical trials, and specialized care approaches. Features insights from the Genetic Eye Disease Center at Johns Hopkins.
- Key Information Used: Genetic testing recommendations, NAC Attack clinical trial details, inheritance patterns, and nutritional precautions, including vitamin E limitations.
3. Foundation Fighting Blindness – Research Advances
- URL: https://www.fightingblindness.org/news/retinitis-pigmentosa-research-advances-899
- Description: Current developments in retinitis pigmentosa treatment research, including gene therapy trials, stem cell studies, and optogenetic approaches. Regularly updated with breakthrough clinical trial results.
- Key Information Used: MCO-010 gene therapy progress, clinical trial enrollment information, emerging treatment pipelines, and research funding developments.
Professional Organizations and Support Resources
- American Academy of Ophthalmology: https://www.aao.org/eye-health/diseases/what-is-retinitis-pigmentosa
- International Academy of Low Vision Specialists: https://ialvs.com/
- ClinicalTrials.gov: https://clinicaltrials.gov/ (Search: “retinitis pigmentosa”)
- Orphanet – Rare Disease Database: https://www.orpha.net/en/disease/detail/791
Looking Forward: Hope and Future Directions
Emerging Treatment Pipeline
The landscape for RP treatment is rapidly evolving:
Gene Therapies: Nanoscope Therapeutics, the developer of MCO-010, is preparing to submit a Biologics License Application to the FDA in early 2025
Stem Cell Advances: Following positive end-of-study results from the RESTORE Phase 2b multicenter, randomized, double-masked, sham-controlled clinical trial for RP
Optogenetic Innovation: Multiple companies are developing light-sensitive proteins to restore vision
Reasons for Optimism
MCO-010 eliminates the need for external devices, simplifying treatment and expanding usability, representing the next generation of vision restoration therapies.
Research Momentum:
- Increased funding for rare disease research
- Advanced understanding of genetic mechanisms
- Collaboration between research institutions and biotech companies
- Patient advocacy driving research priorities
Key Takeaways for Living Well with Retinitis Pigmentosa
Immediate Action Steps:
- Seek comprehensive eye care from retinal specialists experienced with inherited retinal diseases
- Consider genetic testing to understand your specific type and inheritance pattern
- Explore low vision services and assistive technologies through certified specialists
- Connect with support communities and patient advocacy organizations
- Stay informed about clinical trial opportunities and emerging treatments
For Seattle-Area Patients:
- Schedule comprehensive retinal evaluations with specialists familiar with retinitis pigmentosa
- Inquire about genetic counseling services and family planning considerations
- Ask about participation in clinical trials and research studies
- Explore low vision rehabilitation services and assistive technology training
At Cannon EyeCare, we understand the complex challenges faced by patients with inherited retinal diseases. Our comprehensive approach combines advanced diagnostic technologies with personalized care planning, helping patients and their families navigate the journey from diagnosis through long-term management.
Long-term Planning:
- Develop adaptive strategies for daily activities
- Plan career accommodations and transportation alternatives
- Build strong support networks with family and professionals
- Consider genetic counseling for family planning
- Maintain hope while staying realistic about progression
Remember: While no one can predict how much vision you’ll lose or how fast, it’s safe to expect that you’ll need to learn new ways of doing things. Adapting to vision loss can be hard, especially in the middle of your life. But once you’ve made the necessary changes, they’ll become your new normal
With proper medical care, appropriate assistive technologies, strong support systems, and emerging treatment options, individuals with retinitis pigmentosa can continue to lead fulfilling, independent lives while contributing to the research that will benefit future generations.
This comprehensive guide provides current information about retinitis pigmentosa based on the latest medical research and clinical developments. Always consult with qualified eye care professionals for personalized medical advice and treatment decisions.
FAQs
-
-
Retinitis Pigmentosa is a genetic eye disorder causing gradual loss of night and side vision, eventually leading to tunnel vision or blindness.
-