Optic Neuritis
Optic neuritis can cause sudden vision loss and eye pain—do you know the warning signs? Discover what triggers it, how it’s diagnosed, and what recovery looks like.
Key Takeaways: Optic Neuritis in Seattle
-
Optic neuritis causes sudden vision loss and eye pain, primarily due to inflammation of the optic nerve’s myelin sheath—early diagnosis is crucial to prevent long-term damage.
-
Women aged 20–40 in northern regions like Seattle are at significantly higher risk, with vitamin D deficiency and genetic factors contributing to prevalence.
-
Eye movement pain, color desaturation, and central vision loss are hallmark symptoms—prompt medical evaluation is essential when these signs appear.
-
Accurate diagnosis requires a combination of clinical exams, OCT imaging, MRI, and antibody testing to identify subtypes like MS, NMOSD, and MOGAD.
-
High-dose IV steroids within 14 days of onset remain the gold-standard treatment, with plasma exchange and emerging neuroprotective therapies used for severe or resistant cases.
-
Recovery may take up to 12 months, with color vision typically improving first. Milder initial symptoms and early treatment predict better outcomes.
-
50% of patients with optic neuritis develop MS within 15 years—MRI findings and cerebrospinal fluid markers help assess individual risk.
-
Lifestyle modifications for heat sensitivity, tech use, and driving in Seattle’s climate can improve quality of life during recovery.
-
Ongoing care at Seattle’s Cannon EyeCare includes annual MRIs, neurological assessments, and vision rehabilitation support.
-
Vitamin D optimization, smoking cessation, and stress management are key to reducing recurrence and supporting long-term neurological health.
What is Optic Neuritis?
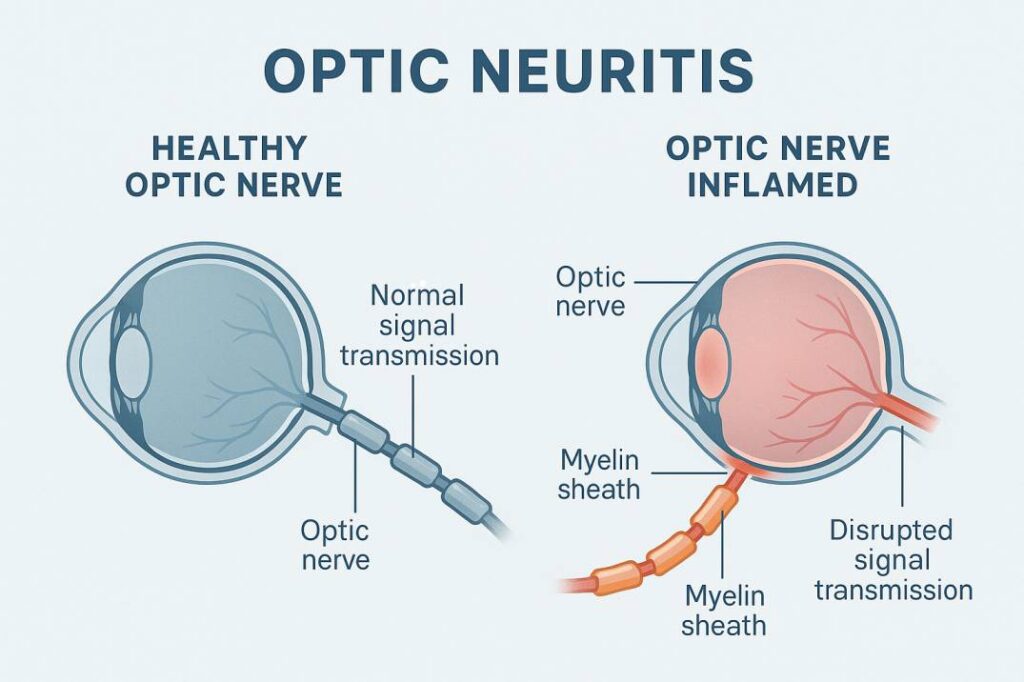
Optic neuritis involves inflammation of the optic nerve—the essential pathway transmitting visual data from your eyes to your brain. Imagine this nerve as a high-speed fiber-optic cable linking your eye’s “lens” to your brain’s “processor.” Inflammation disrupts this connection, causing vision issues and discomfort.
This condition primarily damages the myelin sheath, a protective nerve coating that enables rapid signal transmission. When inflamed, visual signals slow or stop completely.
Types of Optic Neuritis
Eye care professionals categorize optic neuritis into four primary forms:
-
Multiple Sclerosis (MS)-associated: The most common type, affecting 50% of MS patients.
-
Neuromyelitis Optica (NMOSD): Often more severe, typically impacting both eyes.
-
MOG Antibody Disease (MOGAD): A newly identified subtype with unique traits.
-
Isolated optic neuritis: Occurs independently of autoimmune conditions.
Demographics and Risk Factors in Seattle
In Seattle and the broader Pacific Northwest, optic neuritis prevalence reveals key patterns:
-
Women face 3–5x higher risk than men.
-
Most cases occur in adults aged 20–40.
-
Higher rates among Caucasian populations.
-
Northern latitudes (like Seattle’s) correlate with increased incidence.
Recognizing Optic Neuritis Symptoms: Key Warning Signs
Understanding optic neuritis symptoms enables timely intervention and prevents permanent vision damage. At Cannon EyeCare in Seattle, patients consistently report these early warning signs during consultations:
Primary Visual Symptoms
Sudden vision loss is the hallmark symptom, typically developing over hours to days, not gradually. Patients often describe their vision as:
-
“Viewing through frosted glass or Vaseline”
-
“A gray or black spot in the center of vision”
-
“Colors appearing washed out or faded”
-
“Difficulty reading or seeing fine details”
Central scotomas (blind spots in central vision) affect 90% of cases. Unlike peripheral vision loss, these make daily tasks like reading, driving, and recognizing faces especially challenging for Seattle residents.
Pain and Discomfort Patterns
Eye movement pain occurs in 87-92% of optic neuritis cases. This distinct symptom usually:
-
Intensifies when looking up, down, or sideways
-
Feels like a dull ache behind the eye
-
Peaks 3-5 days after onset
-
Often subsides before vision recovery begins
Light sensitivity (photophobia) is common, making bright environments—such as Seattle’s sunny summer days—particularly uncomfortable.
Color Vision Changes
Dyschromatopsia (altered color perception) is a subtle but critical early indicator. Patients may experience:
-
Reduced vibrancy in reds
-
Trouble distinguishing similar shades
-
Overall color “desaturation”
-
Persistent color issues even after vision sharpness returns
When to Seek Emergency Eye Care in Seattle
Contact Cannon EyeCare or seek immediate medical attention if you experience:
-
Sudden vision loss in one or both eyes
-
Severe eye pain worsening with movement
-
Complete central vision loss
-
Bilateral symptoms (affecting both eyes simultaneously)
How Optic Neuritis is Diagnosed
Accurate diagnosis requires a comprehensive approach combining clinical expertise, advanced imaging, and specialized testing. At Cannon EyeCare in Seattle, our specialists utilize cutting-edge diagnostic technology for precise assessment and treatment planning.
Initial Clinical Examination
Your Seattle ophthalmologist performs:
-
Visual acuity testing measures distance vision clarity (often impaired to 20/200 or worse)
-
Pupillary light reflex exam detecting relative afferent pupillary defect (RAPD) – a hallmark sign
-
Fundoscopic evaluation examining optic disc appearance (65% appear normal initially; some show swelling)
Advanced Diagnostic Testing
Optical Coherence Tomography (OCT) delivers high-resolution retinal nerve imaging to:
-
Detect early nerve fiber damage
-
Track treatment effectiveness
-
Predict long-term vision outcomes
-
Differentiate between optic neuritis subtypes
Visual field testing maps peripheral vision loss patterns common in optic neuritis:
-
Central/centrocecal scotomas
-
Temporal defects
-
Superior/inferior field cuts
MRI scans serve critical roles by:
-
Confirming optic nerve inflammation
-
Identifying MS-related brain lesions
-
Ruling out alternative causes
-
Guiding treatment protocols
Specialized Blood Testing
Advanced antibody testing at Seattle clinics identifies subtypes:
-
AQP4 antibodies: Indicate NMOSD (requires distinct treatment)
-
MOG antibodies: Reveal MOGAD with unique management needs
Preparing for Your Seattle Diagnostic Visit
Maximize appointment effectiveness by:
-
Documenting symptom onset/progression
-
Listing all medications/supplements
-
Noting family autoimmune history
-
Bringing previous eye records (Seattle patients can request digital transfers)
Treatment Options for Optic Neuritis: Comprehensive Care Approaches
Modern optic neuritis treatment focuses on reducing inflammation, accelerating recovery, and preventing relapses. At Cannon EyeCare in Seattle, our specialists follow evidence-based protocols while tailoring plans to your unique needs.
Acute Treatment Protocols
High-dose IV corticosteroids remain the gold standard, per the Optic Neuritis Treatment Trial (ONTT):
-
Methylprednisolone (1000mg IV daily for 3–5 days)
-
Oral prednisone taper post-IV therapy
-
Treatment initiation within 14 days of symptoms for optimal results
This approach:
-
Speeds visual recovery in the first 2–3 months
-
Reduces nerve inflammation/swelling
-
May lower short-term MS conversion risk
Note: Oral steroids alone are avoided—they increase recurrence risk without better outcomes.
Alternative Treatments
Plasma exchange (plasmapheresis) helps Seattle patients with:
-
Steroid-unresponsive cases
-
Bilateral vision loss
-
NMOSD-related optic neuritis
Emerging neuroprotective therapies in trials:
-
Phenytoin: Shields nerve fibers
-
Erythropoietin: Promotes nerve repair
-
Memantine: Blocks toxic glutamate effects
Subtype-Specific Strategies
-
NMOSD-associated:
-
Immediate high-dose IV steroids
-
Plasma exchange for severe cases
-
Long-term immunosuppression
-
-
MOGAD-associated:
-
Extended IV steroid courses
-
Gradual tapers to prevent rebound
-
Maintenance therapy for recurrences
-
Managing Treatment Side Effects
High-dose steroids may cause:
-
Sleep disturbances/mood changes
-
Temporary weight gain
-
Blood sugar spikes
-
Gastric irritation
Seattle patients receive proactive monitoring:
-
Glucose checks for diabetics
-
Blood pressure tracking
-
Bone density screening
-
Psychological support resources
Preparing for Treatment in Seattle
-
Discuss activity modifications (e.g., adjusting hiking/routine during therapy)
-
Request vitamin D testing (critical in Pacific Northwest climates)
-
Inquire about telemedicine follow-ups
Recovery Timeline: Navigating Your Healing Journey
Understanding optic neuritis recovery helps Seattle patients maintain realistic expectations while actively supporting healing. Though recovery varies, these general milestones provide guidance:
Acute Phase (Days 1-14)
-
Vision may continue declining for several days after treatment starts—this doesn’t mean treatment failed
-
Eye movement pain typically peaks around days 3-5, then eases
-
IV steroids from Cannon EyeCare usually reduce inflammation markers within 7 days
Early Recovery (Weeks 2-8)
-
Visual improvements often begin 2-3 weeks post-onset
-
Color vision typically returns first
-
Central blind spots gradually shrink (some may persist minimally)
Long-Term Recovery (3-12 Months)
-
Most significant gains occur within the first 3 months
-
Maximum recovery is usually achieved by 12 months
-
Some patients experience lingering effects:
-
Subtle color differences
-
Reduced contrast sensitivity
-
Uhthoff’s phenomenon (vision changes with heat/exertion)
-
Mild visual field gaps
-
Recovery Influencers
-
Age: Better outcomes typically under age 40
-
Initial vision: Less severe loss often means better recovery
-
Treatment timing: Early steroid therapy speeds improvement
-
Subtype: MOGAD/isolated cases often outperform NMOSD
Recovery Enhancement Strategies at Cannon EyeCare
Vision Rehabilitation
-
Contrast-enhancement techniques
-
Visual scanning training
-
Low-vision aid assessments
Lifestyle Adjustments
-
Moderate exercise (avoid overheating)
-
Stress reduction practices
-
Vitamin D supplementation (especially important in our Pacific Northwest climate)
Managing Heat Sensitivity
-
Use cooling accessories during Seattle’s warmer months
-
Modify outdoor activities
-
Maintain cool indoor environments
The Multiple Sclerosis Connection: Navigating Your Risk
Understanding the link between optic neuritis and multiple sclerosis empowers Seattle patients to make informed decisions about monitoring and treatment.
MS Risk Assessment
Following initial optic neuritis:
-
50% develop MS within 15 years
-
High-risk patients (abnormal brain MRI): 72% MS risk
-
Low-risk patients (normal brain MRI): 25% MS risk
Pacific Northwest factors influencing risk:
-
Higher MS prevalence at northern latitudes
-
Regional vitamin D deficiency patterns
-
Genetic factors in local populations
Key MS Predictors
-
Brain MRI: ≥3 white matter lesions = significantly elevated risk
-
Cerebrospinal fluid: Oligoclonal bands (60-70% of future MS patients)
-
Clinical features:
-
Female patients aged 20-40
-
Mild initial vision loss
-
Absence of optic disc swelling
-
Disease-Modifying Therapy Options
Early Treatment Considerations:
-
Pros: Prevents second attacks/reduces disability
-
Cons: Medications carry side effects; not all high-risk patients develop MS
Current Recommendations:
-
Close monitoring via Cannon EyeCare’s Seattle team
-
Treatment initiation upon the second clinical episode or MRI progression
Monitoring Protocols for Seattle Patients
-
Annual MRI surveillance
-
Neurological exams detect subtle changes
-
Symptom education for early recognition:
-
Limb numbness/tingling
-
Muscle weakness
-
Balance issues
-
Unexplained fatigue
-
Proactive Steps at Cannon EyeCare
-
Vitamin D testing (critical in our climate)
-
Personalized risk assessment
-
Coordination with Seattle MS specialists
Living with Optic Neuritis: Practical Seattle Strategies
Adapting to life after optic neuritis involves tailored strategies for Seattle’s active, tech-driven lifestyle. Cannon EyeCare helps patients navigate these changes with confidence.
Managing Residual Vision Changes
For Seattle’s Tech Professionals:
-
Enlarge fonts + use dark mode/high-contrast displays
-
Apply the 20-20-20 rule (20-second screen breaks every 20 minutes)
-
Position monitors at eye level to reduce strain
-
Blue-light glasses for photophobia
Driving Safely in Seattle:
-
Regular vision tests at Cannon EyeCare
-
Avoid I-5/SR-520 during sunrise/sunset glare
-
Polarized sunglasses for highway driving
-
Discuss restrictions with your provider
Heat Sensitivity Management
Combat Uhthoff’s phenomenon during Seattle’s warm months:
-
Cooling towels at Green Lake or Discovery Park walks
-
Early morning kayaking on Lake Union
-
Climate-controlled gym workouts (e.g., Seattle YMCA)
-
Hydration packs for hiking Rattlesnake Ledge
Workplace Accommodations
Under ADA guidelines, request:
-
Large monitors + task lighting
-
Screen-reading software (e.g., JAWS)
-
Flexible remote-work options during flare-ups
-
Adjusted schedules for medical appointments
Seattle Support Resources
-
National MS Society (NW Chapter):
-
Virtual/in-person support groups
-
Financial aid for treatment
-
-
Local Vision Rehabilitation:
-
Low-vision specialists at UW Medicine
-
Assistive tech training
-
-
Mental Health Support:
-
Swedish Medical Center neuro-counseling
-
Mindfulness programs at SAM
-
Emotional Wellness Strategies
Address anxiety/depression with:
-
Therapy specializing in chronic illness (Seattle Anxiety Specialists)
-
Peer groups at Cannon EyeCare’s quarterly meetups
-
Family education sessions
-
Forest bathing in Washington Park Arboretum
Prevention and Long-Term Monitoring Strategies
While primary prevention of optic neuritis is limited, Seattle patients can significantly reduce recurrence risks and protect neurological health through proactive measures at Cannon EyeCare.
Risk Reduction for Pacific Northwest Residents
-
Vitamin D Optimization (critical in our climate):
-
Target: 30-50 ng/mL blood levels
-
Supplementation: 1,000–2,000 IU daily
-
Local testing: Annual screenings at Seattle labs
-
Dietary sources: Wild-caught salmon (Pike Place Market favorites!)
-
-
Smoking Cessation:
-
60% lower recurrence risk for quitters
-
Access Seattle cessation programs (e.g., Swedish Tobacco Program)
-
-
Stress Management:
-
Mindfulness classes at SAM or UW
-
Prioritize 7–9 hours of sleep
-
Join Green Lake walking groups
-
Disease-Modifying Therapies
For MS-associated cases, personalized options include:
-
Self-administered injectables: Interferon beta, glatiramer acetate
-
Oral medications: Dimethyl fumarate, fingolimod
-
Infusion therapies: Ocrelizumab (available at Seattle infusion centers)
Long-Term Monitoring at Cannon EyeCare
Annual exams include:
-
Full neurological + vision testing
-
Brain/spine MRI
-
Cognitive screening
-
Quality-of-life assessment
Interim monitoring:
-
Symptom-triggered evaluations
-
Medication side-effect checks
-
Telehealth consults
Emerging Research
Pacific Northwest clinical trials focus on:
-
Neuroprotection: Growth factor therapies
-
Remyelination:
-
Stem cell applications (UW Medicine trials)
-
Myelin repair drugs
-
Bioengineering approaches
-
Optic neuritis is more than just a temporary eye issue—it can signal deeper neurological concerns and significantly impact daily life if left unaddressed. Early detection, personalized treatment, and consistent follow-up care are essential for preserving vision and preventing long-term complications, especially for patients in high-risk areas like Seattle.
Take control of your eye health today.
If you’re experiencing vision changes or want a personalized risk assessment, schedule a comprehensive evaluation with Cannon EyeCare. Our Seattle specialists are here to guide you through every step—from diagnosis to recovery.
FAQs
-
Optic neuritis causes central blur, like looking through frosted glass or Vaseline on a camera lens, with colors appearing washed out and faded