Ocular Migraine: A Medical Guide to Visual Migraines
The sudden onset of flashing lights, geometric patterns, or temporary vision loss in one eye represents one of medicine’s most misunderstood neurological phenomena. Ocular migraines affect millions worldwide, yet many patients and healthcare providers struggle with accurate diagnosis and management of this condition.
This evidence-based guide synthesizes current medical literature, clinical research, and expert recommendations to provide a comprehensive understanding of ocular migraines—from pathophysiology to practical management strategies.
Clinical Summary: Ocular migraines manifest as transient monocular visual disturbances, including scotomas, scintillating patterns, and temporary blindness, typically resolving within 5-60 minutes. While generally benign, proper differential diagnosis remains essential to exclude serious vascular or neurological pathology.
Clinical Definition and Pathophysiology
Terminology and Classification
Ocular migraine, synonymous with retinal migraine in contemporary medical literature, represents a distinct subset of migraine disorders characterized by transient monocular visual phenomena. The International Classification of Headache Disorders, Third Edition (ICHD-3) defines retinal migraine as “repeated attacks of monocular visual disturbance, including scintillations, scotomata, or blindness, associated with migraine headache.”
The condition differs fundamentally from migraine with aura, which presents bilateral visual symptoms originating from cortical spreading depression. This distinction carries significant clinical implications for differential diagnosis and therapeutic management.
Epidemiological Considerations
Current epidemiological data from 2024-2025 indicate that migraine disorders affect approximately 17-20% of women and 6-7% of men annually, with retinal migraines representing a rare subset of this population. Women demonstrate a 3-4-fold higher prevalence, attributed primarily to hormonal influences, particularly estrogen fluctuations during reproductive years.
Clinical Presentation and Symptomatology
Primary Visual Manifestations
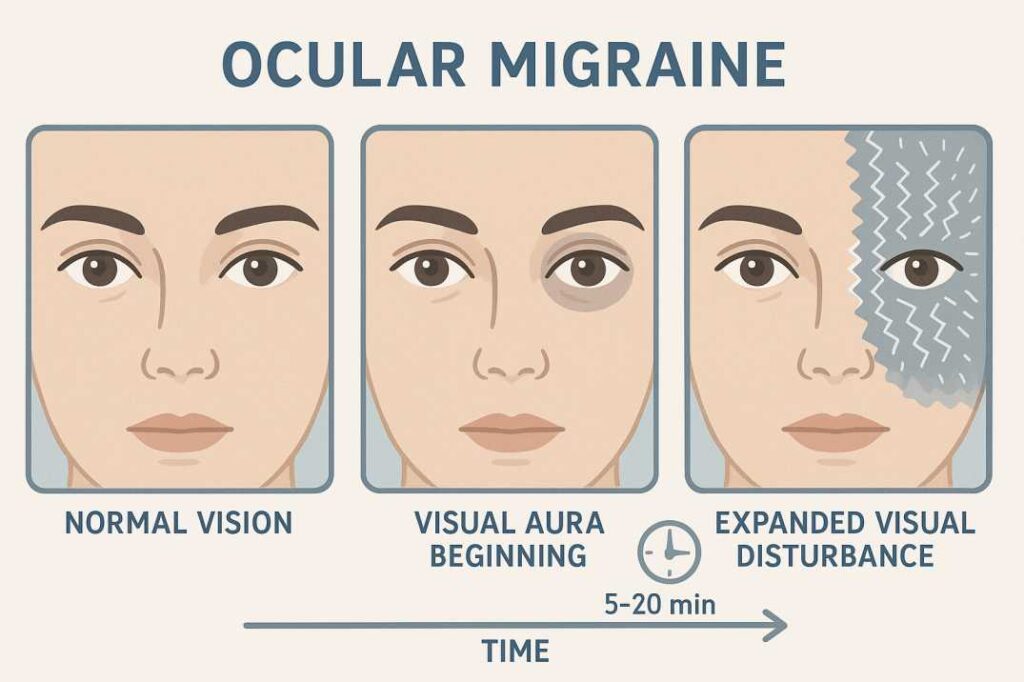
The hallmark feature of retinal migraine involves transient monocular visual disturbances presenting in characteristic phases. Clinical observation reveals a predictable temporal progression:
Initial Phase (0-5 minutes): Patients typically report a small paracentral or central scotoma, often described as a “gray spot” or “blind area” that may shimmer or scintillate.
Expansion Phase (5-20 minutes): The scotoma progressively enlarges, frequently accompanied by positive visual phenomena including geometric patterns (commonly described as “fortification spectra” or “zigzag lines”), scintillating lights, or chromatic disturbances.
Resolution Phase (20-60 minutes): Visual symptoms gradually abate, with complete return to baseline visual function. Concurrent or subsequent cephalgia may develop, typically ipsilateral to the affected eye.
Associated Neurological Symptoms
Contemporary clinical studies demonstrate that visual symptoms occur in isolation in approximately 30% of cases. When present, associated features include:
- Cephalgia (present in 70-75% of cases, typically unilateral)
- Photophobia and phonophobia
- Nausea and emesis
- Transient cognitive symptoms (anomia, dysgraphia)
- Mild hemiparesis (rare, requires exclusion of more serious pathology)
Pathophysiological Mechanisms and Etiology
Vascular vs. Neural Theories
The pathophysiology of retinal migraine remains incompletely understood, with two predominant theories explaining the clinical phenomenon:
Vascular Hypothesis: This theory proposes transient vasoconstriction of retinal or ciliary circulation, resulting in ischemic visual symptoms. Fluorescein angiography during acute episodes has demonstrated delayed filling or occlusion of central retinal artery branches, supporting this mechanism.
Neural Spreading Depression Theory: Alternative models suggest retinal spreading depression analogous to cortical mechanisms in classical migraine aura. This hypothesis proposes that abnormal neuronal depolarization waves propagate across retinal tissues, generating characteristic visual phenomena.
Genetic Predisposition
Contemporary research demonstrates significant familial clustering, with 50% of affected individuals reporting family histories of migraine disorders. Recent genome-wide association studies have identified potential susceptibility loci, though specific genetic markers for retinal migraine remain under investigation.
Precipitating Factors and Triggers
Clinical studies identify multiple precipitating factors consistent with classical migraine triggers:
Physiological Stressors: Emotional stress, sleep disruption, hormonal fluctuations (particularly estrogen withdrawal), physical exertion, altitude changes, and dehydration.
Environmental Factors: Bright or flickering lights, fluorescent illumination, barometric pressure changes, and excessive screen exposure.
Dietary Triggers: Alcohol consumption, aged cheeses, processed meats containing nitrates, chocolate, and artificial sweeteners.
Pharmacological Triggers: Oral contraceptives, vasodilators, and certain antihypertensive medications.
Differential Diagnosis and Clinical Assessment
Diagnostic Challenges
Retinal migraine represents a diagnosis of exclusion, requiring systematic evaluation to eliminate more serious pathological processes. The transient nature of symptoms often precludes direct observation during acute episodes, necessitating reliance on detailed clinical history and temporal pattern recognition.
Essential Differential Considerations
Vascular Etiologies:
- Amaurosis fugax secondary to carotid artery disease
- Central retinal artery occlusion or branch occlusions
- Giant cell arteritis with associated anterior ischemic optic neuropathy
- Vertebrobasilar insufficiency with posterior circulation involvement
Inflammatory/Autoimmune Conditions:
- Multiple sclerosis with optic neuritis
- Neuromyelitis optica spectrum disorders
- Systemic lupus erythematosus with CNS involvement
Structural/Mechanical Causes:
- Angle-closure glaucoma with intermittent pressure elevation
- Papilledema with transient visual obscurations
- Retinal detachment with peripheral involvement
Clinical Assessment Protocol
History Taking: Detailed characterization of visual phenomena, temporal patterns, associated symptoms, family history, and trigger identification remains paramount. Specific attention should be directed toward onset age, episode frequency, and relationship to potential precipitating factors.
Ophthalmological Examination: Comprehensive evaluation including visual acuity, visual field testing, pupillary assessment, fundoscopy, and intraocular pressure measurement. During asymptomatic periods, examination findings typically remain normal.
Neurological Assessment: Basic neurological screening to exclude focal deficits, with particular attention to signs suggesting posterior circulation involvement or increased intracranial pressure.
Who Gets Ocular Migraines? Demographics and Risk Factors
Age and Gender Patterns
Ocular migraine can start as early as 7 years of age. But most people start experiencing them in their 20s, with a peak age of 40. Understanding these demographic patterns can help with early recognition and treatment.
Age Distribution:
- Can begin in childhood (as early as age 7)
- Most common onset: 20s
- Peak incidence: 30-40 years old (updated from previous data showing peak at 40)
- It can occur at any age throughout life
Gender Differences: Like other types of migraines, ocular migraines show a clear gender preference. According to 2025 data, migraines affect approximately 17-20% of women and 6-7% of men annually. Not everyone who has migraines experiences ocular migraines.
Risk Factors
Primary Risk Factors:
- Family history of migraines
- Female gender
- Reproductive age in women
- History of other migraine types
Secondary Risk Factors:
- High stress levels
- Irregular sleep patterns
- Hormonal fluctuations
- Certain medications
- Environmental sensitivities
Recent Research: What Science Tells Us About Ocular Migraines
Clinical Study Findings
Recent research from 2024 published in peer-reviewed journals provides updated insights into ocular migraines. Based on a study by Pradhan et al., it was found that 50% of retinal migraine patients said the vision loss was complete in one eye, up to 20% said it was just blurring, 12% reported an incomplete loss, 7% dimming, and 13% scotoma. More than 75% of patients had a headache on the same side as the vision disturbance within an hour.
Additionally, current data show that 29% of retinal migraine patients have a history of migraine headache, and 50% have a family history of migraine headache, reinforcing the strong genetic component.
Global Trends and Updated Data
According to the most recent global health data from 2024-2025, migraine prevalence has been steadily increasing worldwide. Current estimates show that migraines affect more than 39 million Americans, with global figures indicating that approximately 1.16 billion people worldwide experience migraines. While overall numbers remain higher in women, the rate of increase has been more rapid among men – possibly due to lifestyle changes, improved diagnosis, or better reporting.
Recent research published in 2024 found “Increased risks of retinal vascular occlusion in patients with migraine and the protective effects of migraine treatment” in a population-based study. This research suggests that people with migraines, including ocular migraines, may have increased risks of retinal blood vessel problems, emphasizing the importance of proper treatment and monitoring.
Structural Changes in the Eye
Studies using optical coherence tomography have found that “the mean RNFL thickness for nasal and nasal inferior sectors was significantly thinner in the migraineurs’ eyes than in those of the controls, as was the mean choroid thickness at the fovea.” This research indicates that chronic migraines may cause subtle structural changes in the eye, though the clinical significance of these changes is still being studied.
Therapeutic Management and Clinical Interventions
Acute Episode Management
Immediate Interventions: During acute episodes, patients should discontinue visually demanding activities and seek environmental modifications, including reduced ambient lighting and auditory stimuli. Complete rest remains paramount until visual symptoms fully resolve.
Pharmacological Interventions: Traditional migraine abortive therapies demonstrate variable efficacy in retinal migraine. Triptans, while effective for classical migraine, may paradoxically prolong visual symptoms due to their vasoconstrictive properties and are generally contraindicated during acute visual episodes.
Acute pharmacological management focuses on:
- Non-steroidal anti-inflammatory drugs (NSAIDs) for associated cephalgia
- Antiemetic agents for concurrent nausea and emesis
- Analgesics for pain management post-resolution
Preventive Strategies
Pharmacological Prevention: For patients experiencing frequent episodes (>4 monthly), preventive therapy should be considered:
- Calcium Channel Blockers: Verapamil demonstrates particular efficacy, presumably through stabilization of vascular reactivity
- Beta-Blockers: Propranolol represents the first-line prevention with established efficacy profiles
- Anticonvulsants: Topiramate and valproic acid show benefit in selected patients
- Low-dose Aspirin: Daily aspirin (75-100mg) may reduce episode frequency through antiplatelet mechanisms
Non-Pharmacological Interventions: Comprehensive trigger identification and avoidance strategies form the foundation of preventive management. Lifestyle modifications include sleep hygiene optimization, stress reduction techniques, regular exercise programs, and dietary modification.
Novel Therapeutic Approaches
CGRP-Targeted Therapy: Calcitonin gene-related peptide inhibitors represent emerging therapeutic options, though specific efficacy data for retinal migraine remain limited. These agents show promise given CGRP’s presence in the retinal vasculature.
Neuromodulation Techniques: External trigeminal nerve stimulation and other neuromodulation approaches demonstrate potential benefits, though larger controlled studies are needed to establish definitive efficacy.
Prognosis and Long-term Outcomes
Clinical Course and Natural History
Retinal migraine typically demonstrates a benign clinical course with excellent long-term visual prognosis. The majority of patients experience complete visual recovery between episodes, though rare cases of permanent monocular visual field defects have been reported in the literature.
Episode frequency varies significantly among individuals, ranging from isolated occurrences to multiple monthly episodes. Many patients report spontaneous improvement over time, with decreased frequency and intensity of attacks as they age, particularly following menopause in women.
Risk Stratification
While generally benign, certain clinical features warrant closer monitoring:
- Age of onset after 50 years requires aggressive evaluation for vascular pathology
- Concurrent cardiovascular risk factors necessitate a comprehensive assessment
- Progressive visual symptoms or incomplete recovery between episodes mandate immediate specialist referral
Complications and Sequelae
Permanent visual loss, while rare, has been documented in approximately 5-10% of cases in some series. This typically manifests as persistent scotomata or peripheral visual field defects. The mechanism likely involves prolonged retinal ischemia exceeding cellular tolerance thresholds.
Clinical Practice Guidelines and Recommendations
Emergency Assessment Criteria
Immediate ophthalmological or neurological evaluation is indicated for:
- Visual symptoms persisting beyond 60 minutes
- Progressive visual loss between episodes
- New-onset symptoms after age 50
- Associated neurological deficits
- Severe headache with atypical characteristics
Monitoring and Follow-up Protocols
Initial Assessment: Comprehensive ophthalmological evaluation including visual field testing, optical coherence tomography, and fundus photography to establish baseline measurements.
Ongoing Management: Regular follow-up intervals determined by episode frequency, with particular attention to trigger identification and preventive strategy effectiveness.
Specialist Referral: Neurology consultation is recommended for patients with frequent episodes (>4 monthly), atypical presentations, or concurrent neurological symptoms.
Future Research Directions
Emerging Diagnostic Technologies
Advanced imaging modalities, including optical coherence tomography angiography, show promise for real-time visualization of retinal perfusion changes during acute episodes. These techniques may provide insights into pathophysiological mechanisms and improve diagnostic accuracy.
Novel Therapeutic Targets
Research into retinal-specific CGRP pathways, neuroinflammation markers, and genetic susceptibility factors continues to evolve. These investigations may yield targeted therapeutic interventions with improved efficacy profiles.
Precision Medicine Approaches
Future treatment paradigms may incorporate genetic testing, biomarker analysis, and individualized trigger profiling to develop personalized management strategies optimizing outcomes while minimizing adverse effects.
Summary: Key Takeaways for Ocular Migraine Management
Essential Points to Remember:
- Ocular migraines cause temporary visual disturbances in one eye only
- Episodes typically last 5-60 minutes with full vision recovery
- Common symptoms include blind spots, zigzag patterns, and flashing lights
- Triggers include stress, bright lights, dehydration, and certain foods
- Medical evaluation is essential to rule out serious conditions
- Treatment focuses on trigger avoidance and symptom management
- Most people experience good long-term outcomes with proper care
Additional Resources and Medical References
For readers seeking more detailed medical information about ocular migraines, these authoritative sources provide comprehensive clinical perspectives:
1. Cleveland Clinic – Ocular Migraine Medical Overview
Link: https://my.clevelandclinic.org/health/diseases/24961-ocular-migraine
Key Information: This resource provides detailed medical definitions, diagnostic criteria, and treatment protocols for ocular migraines. Cleveland Clinic’s comprehensive overview covers the condition’s symptoms, which include temporary blind spots, zigzagging patterns, shimmering lights, and floating lines, typically lasting 10-20 minutes before vision returns to normal. The resource emphasizes that while ocular migraines are rare, they can start as early as age 7, with most people experiencing them in their 20s and peaking around age 40.
2. Mayo Clinic – Expert Medical Guidance on Ocular Migraines
Link: https://www.mayoclinic.org/diseases-conditions/migraine-headache/expert-answers/ocular-migraine/faq-20058113
Key Information: Mayo Clinic clarifies the terminology confusion around “ocular migraine” and explains that headache specialists prefer more specific terms like “migraine with aura” and “retinal migraine”. This resource provides crucial guidance on when to seek immediate medical attention, particularly for visual changes that haven’t been previously evaluated or symptoms that begin after age 50.
3. StatPearls Medical Database – Clinical Research on Retinal Migraines
Link: https://www.ncbi.nlm.nih.gov/books/NBK507725/
Key Information: This peer-reviewed medical resource presents the latest clinical research and evidence-based treatment approaches. The database reports that 50% of retinal migraine patients experience complete vision loss in one eye, while 29% have a personal history of migraine headaches, and 50% have a family history of migraines. The resource emphasizes that retinal migraine diagnosis requires exclusion of other serious conditions and should be evaluated by healthcare professionals immediately if symptoms persist beyond normal duration.
Conclusion: Taking Control of Your Ocular Migraines
Ocular migraines can be disruptive and concerning, but with proper understanding and management, most people can significantly reduce their impact on daily life. The key to successful management lies in:
Early Recognition: Understanding your symptoms and triggers helps you respond quickly and appropriately to episodes.
Professional Care: Working with healthcare providers ensures proper diagnosis and access to effective treatments.
Lifestyle Management: Implementing preventive strategies can reduce both the frequency and severity of episodes.
Ongoing Monitoring: Keeping track of your patterns helps optimize treatment approaches over time.
Remember that while ocular migraines can be alarming, they are typically benign conditions that respond well to appropriate treatment. The prognosis for an ocular migraine is good. The frequency and intensity of the headache typically decrease. However, any new or concerning visual symptoms should always be evaluated by a healthcare professional.
If you’re experiencing visual disturbances that might be ocular migraines, don’t hesitate to consult with an eye care professional or neurologist. With the right approach, you can minimize the impact of ocular migraines and maintain your quality of life.
Schedule Your Comprehensive Eye Exam Today. At Cannon EyeCare, our experienced optometrists provide thorough evaluations for ocular migraines and other vision concerns. We combine Midwestern hospitality with expert medical care, ensuring you receive personalized attention and an accurate diagnosis.
Medical Disclaimer: This article was written by medical content specialists and reviewed for accuracy by eye care professionals. The information provided is for educational purposes only and should not replace professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment of medical conditions.
FAQs
-
An ocular migraine is a temporary visual disturbance affecting one eye, causing blind spots, flashing lights, or zigzag patterns. It typically lasts 10-60 minutes and may occur with or without headache pain.