Nystagmus
What is nystagmus, and how does it impact daily life? This guide explores the causes, symptoms, and breakthrough treatments for involuntary eye movements affecting children and adults in Seattle.
Key Takeaways: Understanding and Managing Nystagmus
-
Nystagmus involves involuntary, rhythmic eye movements that can impair vision, balance, and daily functioning—especially in Seattle’s bright, high-motion environments.
-
Two main types exist: congenital (present at birth) and acquired (from trauma, stroke, or neurological disease); early evaluation is critical for identifying serious causes.
-
Symptoms often go unnoticed until daily life is impacted, including difficulty reading, driving, or navigating stairs due to oscillopsia, depth perception loss, and visual fatigue.
-
Seattle patients often benefit from an integrated care approach, combining optical solutions (e.g., prism lenses), medications (like Gabapentin or Brinzolamide), and advanced diagnostics, including AI-assisted analysis.
-
Lifestyle strategies like adjusting screen settings, using adaptive reading tools, and leveraging Seattle-specific transit and workplace accommodations can drastically improve function and comfort.
-
Children with nystagmus thrive with early interventions, customized educational plans (IEPs), OT support, and confidence-building programs tailored to their unique strengths.
-
Seattle is at the forefront of innovation, with research in gene therapy, robotic-assisted surgery, and mobile eye-tracking apps paving the way for future treatments and personalized care.
What Is Nystagmus? Understanding Involuntary Eye Movements
Nystagmus is an eye condition causing involuntary, rhythmic eye movements that cannot be consciously controlled. Unlike typical eye motions (like reading or tracking objects), these movements are constant and repetitive, creating a distinct “bouncing” or “shaking” sensation in vision.
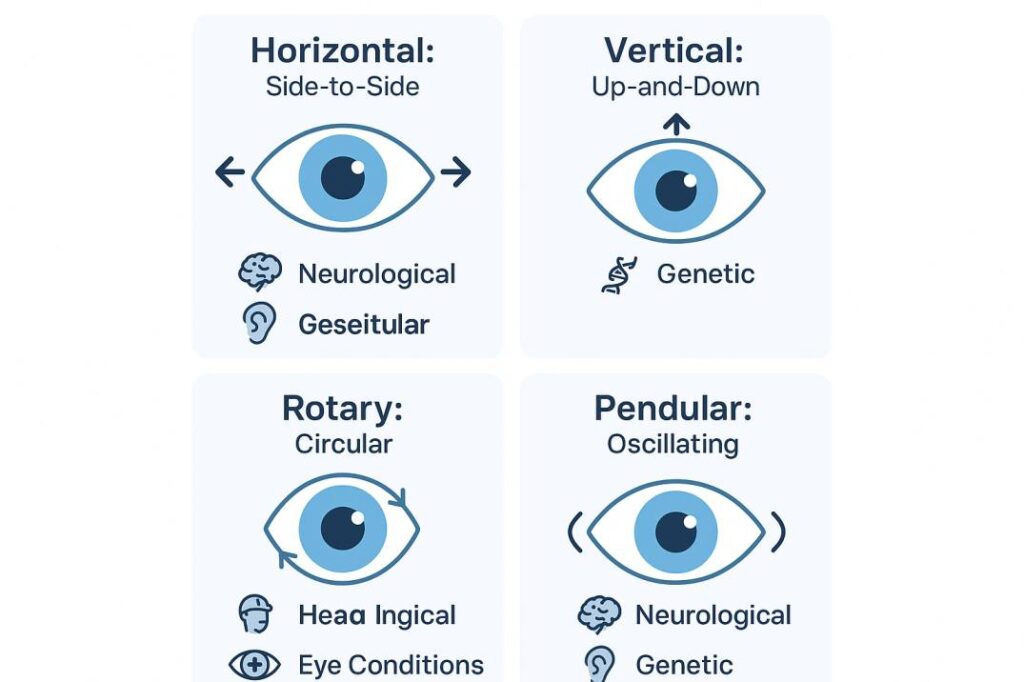
These involuntary movements follow distinct patterns, often described by Seattle patients as a persistent “bouncing” or “shaking” of vision. Common types include:
-
Horizontal: Side-to-side motion (like watching tennis)
-
Vertical: Up-and-down movement (like tracking a bouncing ball)
-
Rotary: Circular motions
-
Mixed: Combination of patterns
Speed and intensity can fluctuate daily, significantly affecting depth perception, balance, and daily activities for those living with nystagmus.
Congenital vs. Acquired Nystagmus: Key Differences
Congenital (Infantile) Nystagmus:
- Appears at birth or in infancy
- Often genetic (runs in families)
- Linked to conditions like albinism or childhood cataracts
- Managed by Seattle pediatric eye care specialists
Acquired Nystagmus:
- Develops later due to head injury, neurological disease, stroke, or medication
- Requires urgent evaluation by a Seattle eye doctor to rule out serious conditions like brain tumors or MS
Common Types of Nystagmus & Movement Patterns
Nystagmus manifests in distinct movement patterns, each requiring specialized evaluation:
Horizontal Nystagmus
-
Most prevalent form (side-to-side eye movements)
-
Seattle patients often adopt unique head positions to stabilize vision
-
Management focuses on vision therapy and corrective lenses
Vertical Nystagmus
-
Less common but clinically significant
-
Upbeat: Eyes drift upward
-
Downbeat: Eyes drift downward
-
Often indicates brainstem issues or neurological disorders requiring urgent Seattle neuro-ophthalmology referral
Rotary (Torsional) Nystagmus
-
Circular eye rotations
-
Strongly linked to inner ear disorders
-
Typically causes vertigo and balance impairment
-
Requires collaboration with Seattle vestibular specialists
Movement Pattern Variations
-
Jerk Nystagmus:
Slow drift in one direction + rapid corrective “jerk” -
Pendular Nystagmus:
Equal-speed swinging motions (like a pendulum)
Recognizing Nystagmus Symptoms: Patient Experiences in Seattle
Many individuals with nystagmus adapt to their eye movements as normal, yet these symptoms significantly impact daily life:
Core Visual Challenges
-
Oscillopsia: Persistent sensation of the world bouncing or shaking
-
Reduced Visual Acuity: Blurred vision, especially for distant objects
-
Impaired Depth Perception: Difficulty judging stairs, distances, or spatial relationships
-
Photophobia: Worsened symptoms in bright Seattle daylight or glare
Common Compensatory Strategies
Patients instinctively develop habits to improve focus:
-
Head Positioning: Tilting/turning to find the “null point” (minimal movement zone)
-
Visual Adjustments: Squinting, closing one eye, or holding materials at unusual distances
-
Activity Modifications: Avoiding high-motion environments like crowded spaces
Associated Physical & Social Impacts
-
Vertigo/Balance Issues: Especially with rotary nystagmus
-
Eye Strain Headaches: From prolonged visual effort
-
Functional Limitations: Difficulty with driving, reading, or sports
-
Social Discomfort: Anxiety about visible eye movements in social settings
Early evaluation by a Seattle neuro-optometrist helps manage these symptoms and preserve quality of life.
Nystagmus Causes & Risk Factors: Insights from Seattle Practice
Identifying the root cause is essential for effective management. At Cannon EyeCare, we diagnose these common triggers among Seattle patients:
Genetic & Developmental Factors
-
Inherited conditions: Albinism, congenital cataracts, Leber congenital amaurosis
-
Family history (affects 20-30% of congenital cases)
-
Syndromes: Down syndrome, neurofibromatosis
Neurological Origins
-
Stroke (brainstem/cerebellum)
-
Multiple sclerosis (MS)
-
Brain tumors
-
Head trauma from accidents or sports injuries
Vision-Specific Causes
-
Extreme uncorrected refractive errors
-
Childhood cataracts
-
Adult-onset macular degeneration
-
Optic nerve disorders like optic neuritis
Systemic & Environmental Contributors
-
Medication side effects (anticonvulsants, lithium)
-
Alcohol/drug toxicity or withdrawal
-
Vestibular disorders (e.g., Ménière’s disease)
-
Nutritional deficiencies (B12/thiamine)
Seattle-specific risk factors: Our region’s high MS prevalence and active lifestyle increase exposure to neurological triggers and head injuries.
Nystagmus Diagnosis: Advanced Evaluation at Cannon EyeCare
Early, precise diagnosis directs effective treatment. Our Seattle clinic performs comprehensive evaluations beyond standard eye exams:
Step 1: Personalized Medical History
We explore:
-
Symptom onset timeline
-
Family eye health history
-
Current medications
-
Head injuries or neurological conditions
Step 2: Specialized Testing
-
Eye Movement Analysis: High-speed video recording to map movement patterns
-
Adaptive Visual Acuity: Testing vision at various distances/head positions
-
Enhanced Refraction: Identifying prescription needs that may reduce nystagmus
-
Digital Fundus Exam: Detecting albinism, optic nerve, or retinal issues
Step 3: Advanced Neuro-Visual Diagnostics
-
AI-Assisted Pattern Classification: 70% faster sub-type identification
-
Visual Evoked Potential (VEP): Measures brain visual processing efficiency
-
Collaborative Imaging: Coordination with Seattle imaging centers for MRI/CT scans when neurological causes are suspected
Why Seattle patients choose us: Integrated care from diagnosis to management planning in one location.
Nystagmus Management: Cutting-Edge Treatments at Cannon EyeCare
While nystagmus has no cure, patients in Seattle achieve significant improvements in vision and quality of life through personalized management. Our approach targets your specific type, severity, and root cause:
1. Advanced Pharmaceutical Therapies
-
Brinzolamide Eye Drops: 2024 clinical trials show improved visual acuity and reduced movement severity
-
Oral Medications:
-
Baclofen: Reduces muscle-related nystagmus
-
Gabapentin: Stabilizes acquired cases
-
Memantine: Emerging option for neurological origins
-
2. Precision Optical Solutions
-
Customized Prescription Lenses: Correcting even mild refractive errors to reduce eye strain
-
Prism Lenses: Align images to minimize double vision
-
Medical-Grade Contacts: Enhanced stability vs. glasses
-
Therapeutic Tints: Reduce glare in Seattle’s variable lighting
3. Surgical Interventions
-
Extraocular Muscle Surgery: Repositions eye muscles to:
-
Correct compensatory head postures
-
Improve functional vision
-
-
Seattle Surgical Specialists: Partnering with neuro-ophthalmologists for 79% visual acuity success rates
Why our approach works: Integrated medical, optical, and surgical coordination within Seattle’s specialist network.
Daily Life with Nystagmus: Seattle-Specific Management Strategies
Beyond medical care, these actionable approaches help Seattle residents thrive with nystagmus:
Reading & Close Work Optimization
-
Lighting: Maximize natural light (precious in Seattle!) + task lighting
-
Positioning: Use adjustable reading stands to find your “sweet spot”
-
Tools: Large-print materials, e-readers with font customization
-
Eye Care: Follow the 20-20-20 rule during extended focus
Digital Screen Adaptation
-
Reduce glare with anti-reflective screen filters
-
Enable high-contrast mode/dark themes on devices
-
Position monitors at null-point angles to minimize head turns
-
Use voice-to-text software for lengthy typing
Seattle Workplace Success
Under ADA/Washington State law:
-
Request adjustable lighting/ergonomic seating
-
Utilize magnification software (ZoomText, JAWS)
-
Secure flexible scheduling for low-vision days
-
Access WA State Dept. of Services for the Blind resources
Pacific Northwest Mobility
-
Driving Safety:
-
Regular specialized vision testing at our Seattle clinic
-
Consider bioptic telescopes for road signs
-
Limit night driving in rainy conditions
-
-
Urban Alternatives:
-
Link light rail’s high-contrast signage
-
King County Metro’s Priority Seating program
-
Access Paratransit services
-
Pediatric Nystagmus Support: Empowering Seattle Families
An early nystagmus diagnosis can feel overwhelming, but Seattle children thrive with proactive support. Our approach focuses on ability-centered development:
Educational Success Strategies
Collaborate with schools using IEP/504 Plans:
-
Front-row seating for board visibility
-
Large-print/digital textbooks
-
Extended test time + assistive tech (screen readers)
-
Quarterly teacher meetings to explain compensatory behaviors (head tilting, close viewing)
Key Seattle Resources:
-
Seattle Public Schools Vision Services
-
WA Office of Superintendent of Public Instruction (OSPI)
Confidence-Building Techniques
-
Strength-focused activities: Swimming, hiking, or Seattle’s adaptive sports programs
-
Peer connection: Lighthouse for the Blind family workshops
-
Early self-advocacy training: “My eyes work differently” scripts
-
Celebrate milestones: Customize expectations while encouraging growth
Development & Social Navigation
-
Motor skills: Partner with Seattle pediatric OTs for balance/fine motor support
-
Social prep: Role-play explaining nystagmus to classmates
-
Recreation:
-
Modified sports (Beep Baseball, Goalball)
-
Sensory-friendly Seattle outings (Pacific Science Center quiet hours)
-
Nystagmus Research Breakthroughs: Seattle’s Role in Future Care
The nystagmus treatment landscape is evolving rapidly, with Seattle’s medical research community driving pivotal advances:
AI-Powered Precision Medicine
-
Next-Gen Eye Tracking: Machine learning analyzes subtle movement patterns for personalized treatment plans
-
Home Monitoring Tools: Smartphone apps enable real-time symptom tracking between Seattle clinic visits
-
Local Connection: UW Medicine’s computational neuroscience partnerships
Genetic Therapy Frontiers
-
Target discovery for inherited forms (albinism-related, congenital motor nystagmus)
-
Benaroya Research Institute trials exploring viral vector delivery systems
-
Future potential: Single-treatment interventions for genetic subtypes
Novel Pharmaceutical Pipeline
-
Phase III Trials:
-
Potassium channel blockers (reducing hyperexcitability)
-
GABAergic drugs for cerebellar-related nystagmus
-
-
Cannabinoid Research: CBD/THC formulations for acquired oscillation control
Surgical Advancements
-
Robotic-Assisted Procedures: Sub-millimeter muscle adjustments
-
Adjustable Suture Techniques: Post-op refinement of eye alignment
-
Seattle Children’s Hospital is pioneering minimally invasive pediatric approaches
Resources & citations
Living with nystagmus can present daily challenges—but with the right diagnosis, treatment, and support, clear and stable vision is possible. Whether you’re managing symptoms yourself or seeking help for a loved one, early intervention makes a lasting difference.
Ready to take control of your vision?
Schedule a comprehensive neuro-visual exam at Cannon EyeCare in Seattle today and discover personalized solutions that bring clarity, comfort, and confidence back into focus
FAQs
-
Nystagmus causes involuntary, rhythmic eye movements that you cannot control. Common signs include rapid side-to-side movements, head tilting for clearer vision, and difficulty tracking moving objects.