Hypertension’s Hidden Impact on Eyesight
Understanding how hypertension silently threatens your eyesight and the steps you can take to protect your vision through comprehensive care and early detection.
The Silent Threat to Your Vision
High blood pressure affects nearly 120 million Americans, earning its reputation as a “silent killer” because symptoms often don’t appear until serious damage has occurred. What many people don’t realize is that this condition poses an equally silent threat to their vision. The delicate network of blood vessels in your eyes serves as a unique window into your cardiovascular health—and when blood pressure remains elevated, these vessels bear the brunt of the damage.
Recent data from the Centers for Disease Control and Prevention reveals that high blood pressure was a primary or contributing cause of 664,470 deaths in the United States in 2023. Yet current statistics show that only about one in four adults with hypertension has their condition properly controlled, leaving millions at risk for serious complications, including vision loss.
Understanding the Eye-Hypertension Connection
The relationship between high blood pressure and eye health centers on the intricate vascular system that nourishes your retina. This light-sensitive tissue at the back of your eye requires a steady supply of oxygen and nutrients delivered through microscopic blood vessels. When blood pressure consistently exceeds normal levels, it places excessive stress on these delicate vessels throughout your body, including those serving your eyes.
Think of your cardiovascular system as an intricate network of highways and neighborhood streets. High blood pressure creates traffic congestion that overwhelms the smallest, most vulnerable pathways. Over time, this constant pressure weakens vessel walls, narrows their openings, and can cause them to leak or rupture entirely.
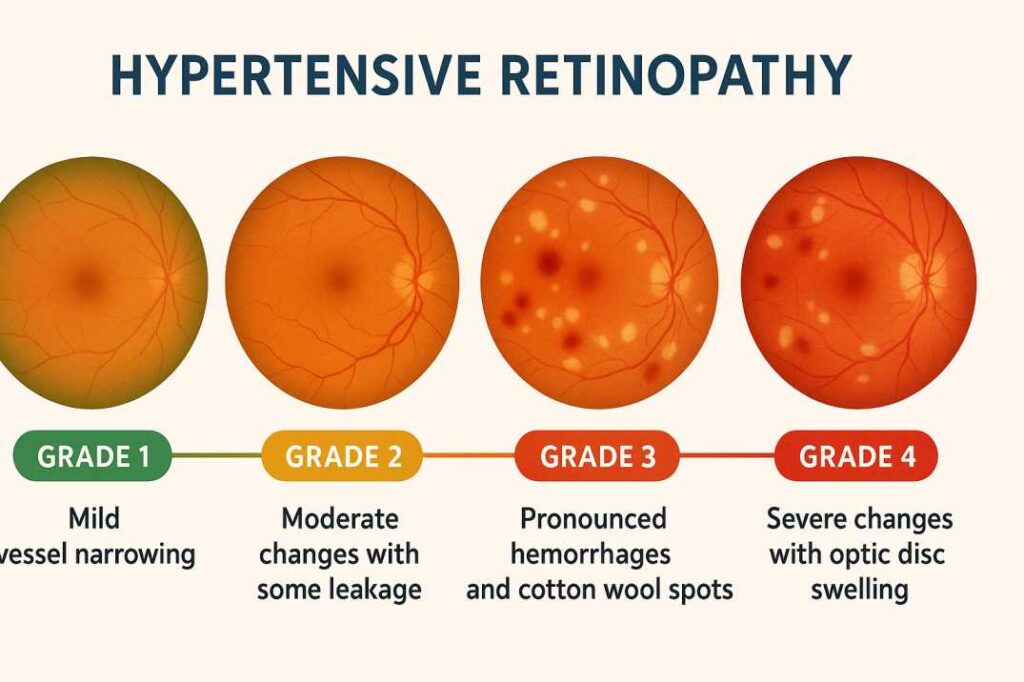
The Progressive Nature of Hypertensive Retinopathy
Hypertensive retinopathy—the medical term for eye damage caused by high blood pressure—develops through predictable stages that often go unnoticed until significant harm has occurred. This progression underscores why regular eye examinations are crucial for anyone with elevated blood pressure.
Grade 1 (Mild): Subtle narrowing of retinal arteries occurs, typically producing no symptoms. Only a comprehensive eye examination can detect these early changes.
Grades 2-3 (Moderate): Blood vessels show more pronounced changes, including increased narrowing, arteriovenous compression, and possible leakage. Patients may still experience no symptoms despite progressive damage.
Grade 4 (Severe): Significant swelling affects the optic nerve and central retina (macula), often causing noticeable vision changes. This stage frequently indicates serious cardiovascular complications requiring immediate medical attention.
Recent research conducted in Northwest Ethiopia involving 696 patients found that 57.47% of individuals with hypertension showed some degree of retinal damage, highlighting the widespread nature of this condition.
Recognizing the Warning Signs
While early-stage hypertensive retinopathy typically produces no symptoms, several warning signs may indicate advancing eye damage from high blood pressure:
Visual disturbances, including temporary blurring, difficulty focusing, or fluctuating vision quality, can signal disrupted blood flow to the retina. These episodes may seem minor, but they often precede more serious complications.
Headaches accompanied by vision changes represent a potentially concerning combination that warrants immediate medical evaluation, particularly in individuals with known hypertension.
Double vision can occasionally result from high blood pressure’s effects on the blood vessels serving the muscles that control eye movement.
Sudden vision changes of any kind—including severe vision loss, flashing lights, or the appearance of a “curtain” across your visual field—require emergency medical care, especially for those with elevated blood pressure.
Beyond Retinopathy: Other Vision Complications
High blood pressure contributes to several additional eye conditions that can threaten vision:
Choroidopathy occurs when fluid accumulates beneath the retina due to damaged blood vessels in the deeper layers of the eye. This condition can cause visual distortion and, in severe cases, permanent scarring.
Optic neuropathy results from inadequate blood flow to the optic nerve, the critical pathway that transmits visual information from your eye to your brain. Damage to this structure can cause partial or complete vision loss.
Retinal vascular occlusions happen when blood clots block the arteries or veins serving the retina. High blood pressure significantly increases the risk of these sight-threatening events, which fall under the broader category of retinal disorders that require immediate medical attention.
Glaucoma risk increases with elevated blood pressure, as higher pressure within the eye can damage the optic nerve over time, leading to gradual vision loss. Glaucoma treatment requires specialized care and regular monitoring.
The Cardiovascular-Vision Risk Connection
Emerging research reveals that eye findings in hypertensive patients correlate strongly with broader cardiovascular risks. A comprehensive meta-analysis of six population-based studies found that even mild hypertensive retinopathy increased cardiovascular disease risk by 13% and coronary heart disease risk by 17%.
A landmark study published in the journal Hypertension tracked nearly 3,000 patients with high blood pressure for 13 years. Those with mild hypertensive retinopathy showed a 35% increased stroke risk, while patients with moderate to severe retinal changes faced a 137% higher risk of stroke.
Special Considerations: Diabetes and Hypertension
The combination of diabetes and high blood pressure creates a particularly dangerous scenario for eye health. High blood pressure compounds the retinal blood vessel damage already caused by elevated blood sugar levels, significantly accelerating the progression of diabetic retinopathy. Patients managing both conditions require more frequent eye monitoring and aggressive treatment of both their blood pressure and blood glucose levels.
The Importance of Comprehensive Eye Examinations
Regular eye examinations serve as a crucial early warning system for both eye and systemic health problems. As Dr. William White, an optometrist with Baylor Scott & White Health, explains, “We can see changes due to vascular conditions caused by diabetes or hypertension. The blood vessels in the retina can become a little stiffer and hardened. They’ll push on each other and cross, like two hoses in a confined space.”
During a comprehensive eye examination, your eye care professional uses specialized instruments to examine your retinal blood vessels directly. This non-invasive process can reveal narrowing, leakage, hemorrhages, and swelling that indicate hypertensive damage.
The recommended examination schedule varies based on your blood pressure control:
- Annual examinations for individuals with well-controlled hypertension
- Every six months for those with uncontrolled blood pressure or existing retinal changes
- Immediate evaluation for any sudden vision changes or symptoms
For those new to eye and vision exams, understanding what to expect can help ensure you receive the most comprehensive care possible.
Treatment and Prevention Strategies
Managing hypertensive retinopathy requires addressing its root cause: elevated blood pressure. A medical eye exam can help determine the extent of any existing damage and guide treatment decisions. The 2025 American Heart Association and American College of Cardiology guidelines emphasize achieving systolic blood pressure below 130 mmHg, with encouragement to reach levels below 120 mmHg when safely possible.
Lifestyle modifications form the foundation of blood pressure management:
Dietary changes following the DASH (Dietary Approaches to Stop Hypertension) eating plan emphasize fruits, vegetables, whole grains, lean proteins, and limited sodium intake. Regular physical activity—at least 150 minutes of moderate-intensity exercise weekly—helps lower blood pressure and supports overall cardiovascular health.
Weight management plays a crucial role, as excess body weight increases the workload on your cardiovascular system. Stress reduction techniques, including meditation, deep breathing exercises, or regular physical activity, can help manage both blood pressure and its effects on eye health.
Avoiding tobacco and limiting alcohol consumption reduces additional cardiovascular stress that can compound hypertensive damage to your eyes.
Medical management often requires prescription medications to achieve target blood pressure levels. The 2025 guidelines emphasize earlier intervention, recommending medication initiation sooner to prevent organ damage. Strict adherence to prescribed treatments is essential, as blood pressure medication only works when taken consistently as directed.
Emergency Situations
Certain symptoms require immediate medical attention, as they may indicate a severe hypertensive crisis affecting your vision:
- Sudden, severe vision loss in one or both eyes
- Sudden onset of double vision
- Severe headaches accompanied by vision changes
- Seeing flashing lights or dark “curtains” across your visual field
- Any rapid onset of visual symptoms in someone with known hypertension
Looking Forward: Prevention and Early Action
The connection between high blood pressure and vision loss represents both a serious health threat and an opportunity for prevention. Unlike many eye conditions, hypertensive retinopathy is largely preventable through proper blood pressure management and regular monitoring.
Some individuals experience improvement in retinal changes after achieving better blood pressure control, though severe damage may be irreversible. This underscores the importance of early detection and intervention before permanent harm occurs.
Current statistics show that about one in four adults with hypertension has their condition under control, leaving significant room for improvement. By understanding the vision implications of high blood pressure and taking proactive steps to manage this condition, individuals can protect not only their cardiovascular health but also their precious gift of sight.
The integration of regular eye care into hypertension management provides a comprehensive approach to health maintenance. Taking time to prepare for your eye exam ensures you get the most value from each visit. As Dr. White notes, “You’re not just a pair of eyeballs walking into an exam room. We have to look at the entire person and the whole picture. These are things that can impact their lives significantly, and we have a responsibility for their overall health.”
Additional Resources and Medical References
American Heart Association – High Blood Pressure Facts
https://www.cdc.gov/high-blood-pressure/data-research/facts-stats/index.html
Current CDC statistics and data on hypertension prevalence, treatment, and control rates in the United States.
International Journal of Retina and Vitreous – Hypertensive Retinopathy Research
https://journalretinavitreous.biomedcentral.com/articles/10.1186/s40942-025-00631-2
Comprehensive 2024 multicenter study examining hypertensive retinopathy prevalence among 696 patients.
2025 AHA/ACC High Blood Pressure Guidelines
https://professional.heart.org/en/science-news/2025-high-blood-pressure-guideline
The most current clinical practice guidelines for prevention, detection, evaluation, and management of high blood pressure in adults.
Conclusion
High blood pressure’s effects extend far beyond cardiovascular complications to threaten one of our most valued senses. The silent progression of hypertensive retinopathy means that vision damage can occur without warning, making regular eye examinations and blood pressure management essential components of comprehensive health care.
With nearly half of American adults affected by hypertension, understanding this connection becomes increasingly important. The encouraging news is that with proper management, many cases of vision loss from high blood pressure are preventable. Taking action today—through lifestyle modifications, medical management, and regular monitoring—can preserve both your cardiovascular health and your vision for years to come.
FAQs
-
High blood pressure damages tiny blood vessels in the retina, causing blurred vision, hemorrhages, and potential permanent vision loss.