Hyperopia
Bottom Line Up Front: Hyperopia affects 30.9% of adults worldwide, making everyday tasks like reading and computer work challenging due to blurry near vision. This evidence-based guide examines hyperopia symptoms, underlying causes, and proven treatment options—from prescription glasses starting at $200 to advanced LASIK surgery. Whether you’re experiencing eye strain during close work or considering vision correction surgery, understanding your options empowers better decisions for lifelong eye health.
Understanding Hyperopia: What Is Farsightedness?
Hyperopia, medically termed farsightedness, represents one of the most common yet misunderstood vision conditions affecting millions worldwide. This refractive error creates a visual paradox where distant objects appear relatively clear while nearby text, screens, and detailed work become frustratingly blurry.
The condition occurs when your eye’s focusing system—specifically the cornea and lens—fails to bend incoming light precisely onto the retina. Instead, light rays converge at a point behind the retina, creating the characteristic blur that defines hyperopic vision. This optical mismatch affects over 75 million Americans and can significantly impact daily productivity, learning, and quality of life.
Clinical Classifications of Hyperopia
Understanding hyperopia’s spectrum helps explain why symptoms vary dramatically between individuals:
Low Hyperopia (+0.25 to +2.00 D). Often asymptomatic in younger patients due to natural accommodation ability. May manifest as occasional eye strain during prolonged near work.
Moderate Hyperopia (+2.25 to +5.00 D)
Typically produces noticeable symptoms, including reading difficulties, digital eye strain, and fatigue. Most patients benefit significantly from corrective intervention.
High Hyperopia (+5.25 D and above) usually requires immediate correction to prevent complications such as amblyopia in children and persistent visual discomfort in adults.
Understanding the Science: How Hyperopia Affects Your Vision
Your eye works like a sophisticated camera, with the cornea and lens acting as focusing elements. In a perfectly functioning eye, these components bend light to create a sharp image directly on the retina at the back of your eye.
With hyperopia, this focusing system is disrupted in two primary ways:
Axial Hyperopia (Most Common)
- The eyeball is shorter than normal from front to back
- Light focuses behind the retina instead of on it
- Usually present from birth due to genetic factors
Refractive Hyperopia (Less Common)
- The cornea or lens lacks sufficient curvature
- Can result from injury, surgery, or certain medical conditions
- The eye’s focusing power is inadequate
Hyperopia Symptoms: Recognizing Farsightedness Signs
Hyperopia presents a complex symptom profile that extends beyond simple vision blur. Understanding these manifestations enables earlier detection and more effective treatment planning.
Primary Visual Symptoms
Near Vision Impairment The hallmark symptom involves progressive difficulty focusing on close objects. Patients often report that small print appears fuzzy, smartphone screens strain their eyes, and detailed work becomes uncomfortable within minutes.
Accommodative Fatigue. Unlike other refractive errors, hyperopia forces the eye’s focusing muscles to work continuously, even for distance vision. This constant accommodation creates a cascade of symptoms, including eye fatigue, burning sensations, and the feeling that eyes are “working too hard.”
Variable Vision Quality Many patients describe fluctuating vision throughout the day, with morning clarity deteriorating into afternoon blur as accommodative muscles tire.
Secondary Symptoms and Complications
Asthenopic Syndrome. This clinical term describes the constellation of symptoms resulting from prolonged accommodative effort:
- Frontal or temporal headaches, particularly after reading or computer work
- General eye discomfort and burning sensations
- Difficulty concentrating on visual tasks
- Neck and shoulder tension from compensatory posturing
Pediatric Presentations Children may exhibit different symptom patterns:
- Frequent eye rubbing or blinking
- Avoidance of reading or homework
- Short attention spans for near tasks
- Holding books or devices at unusual distances
- Academic performance below potential despite normal intelligence
Red Flag Symptoms Requiring Immediate Attention
Certain symptoms warrant urgent evaluation:
- Sudden onset of vision changes
- Severe headaches with visual disturbances
- Eye pain or persistent redness
- Seeing halos around lights
- Partial vision loss or blind spots
Hyperopia Causes and Risk Factors: Why Farsightedness Develops
Hyperopia emerges from a complex interplay of anatomical, genetic, and developmental factors. Understanding these underlying mechanisms provides crucial insights for both prevention strategies and treatment planning.
Anatomical Foundations
Axial Hyperopia (Most Common – 85% of cases) The predominant cause involves an eyeball that measures shorter than the standard 24mm axial length. This shortened anterior-posterior dimension creates insufficient space for proper light convergence on the retinal surface. Even a 1mm reduction in axial length can produce approximately 3 diopters of hyperopia.
Refractive Hyperopia (15% of cases). Less common but equally significant, this variant occurs when corneal curvature or lens power proves inadequate for the eye’s axial length. Contributing factors include:
- Corneal flattening (curvature less than 41 diopters)
- Reduced crystalline lens power
- Anterior chamber depth variations
- Lens position abnormalities
Genetic Architecture and Hereditary Patterns
Modern genetic research has identified multiple loci contributing to hyperopia development:
Inheritance Patterns Hyperopia demonstrates strong familial clustering, with heritability estimates ranging from 0.7 to 0.9. Children with:
- One hyperopic parent: 25-30% risk of developing hyperopia
- Two hyperopic parents: 45-60% risk of developing hyperopia
- Hyperopic siblings: 40% increased risk compared to the general population
Associated Genetic Syndromes Several genetic conditions present with hyperopia as a component:
- Down syndrome (trisomy 21)
- Achromatopsia
- Fragile X syndrome
- Stickler syndrome
- Marfan syndrome (variable presentation)
Environmental and Developmental Factors
Critical Growth Periods Eye development follows predictable patterns, with most children born with mild physiological hyperopia (+2.00 to +3.00 D) that typically resolves through normal growth. Disruption of this emmetropization process can result in persistent hyperopia.
Acquired Causes Though less common, certain conditions can induce hyperopia:
- Lens-induced changes (diabetes, medications)
- Surgical complications (overcorrection in myopia surgery)
- Trauma affecting corneal curvature
- Age-related lens changes (nuclear sclerosis)
Comprehensive Hyperopia Diagnosis: Advanced Assessment Methods
Contemporary hyperopia diagnosis extends far beyond traditional eye charts, incorporating sophisticated technology and evidence-based protocols to ensure accurate measurement and optimal treatment planning.
Gold Standard Diagnostic Protocols
Cycloplegic Refraction The definitive diagnostic procedure temporarily paralyzes accommodation using mydriatic agents (typically cyclopentolate 1% or atropine). This pharmacological approach reveals the eye’s true refractive error by eliminating the confounding effects of accommodative effort—particularly crucial in children and young adults with strong accommodation.
Objective Refraction Techniques
- Autorefraction: Provides rapid initial measurements but may underestimate hyperopia in uncyclopleged patients
- Retinoscopy: Remains the gold standard for objective refraction, offering precise measurements independent of patient cooperation
- Wavefront analysis: Advanced aberrometry identifies higher-order aberrations affecting visual quality
Advanced Diagnostic Technologies
Corneal Topography and Tomography Modern devices map corneal curvature and thickness with micron-level precision, identifying:
- Corneal astigmatism components
- Irregular curvature patterns
- Thickness variations affecting surgical candidacy
Biometry and Axial Length Measurement. Optical coherence interferometry provides accurate axial length measurements, distinguishing between axial and refractive hyperopia subtypes. This information proves crucial for:
- Surgical planning calculations
- Progressive hyperopia monitoring
- Research into emmetropization failure
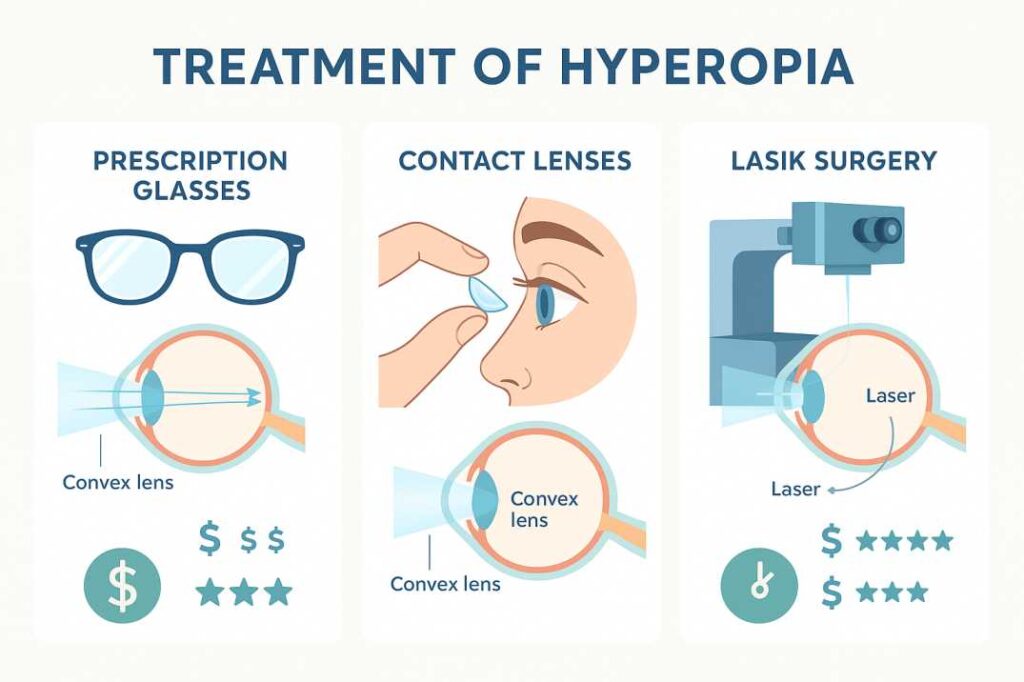
Evidence-Based Hyperopia Treatment Options
Contemporary hyperopia management offers a sophisticated array of interventions, each backed by extensive clinical research and tailored to individual patient needs, lifestyle requirements, and anatomical considerations.
Non-Surgical Interventions
Optical Correction Methods
Prescription Eyeglasses Modern spectacle correction represents the safest, most predictable treatment approach for hyperopia across all age groups.
Clinical specifications:
- Convex lens design with positive dioptric power
- Material options: Standard plastic, polycarbonate, high-index polymers
- Advanced coatings: Anti-reflective, UV protection, blue light filtering
- Cost analysis: $200-$60,0 depending on lens complexity and frame selection
- Success rate: Nearly 100% visual improvement when properly prescribed
Lens design considerations:
- Single-vision lenses for distance and near correction
- Progressive addition lenses (PALs) for presbyopic patients
- Occupational lenses optimized for computer work
- Photochromic options for variable lighting conditions
Contact Lens Correcti: on Contemporary contact lens technology offers excellent hyperopia correction with enhanced comfort and convenience.
Available modalities:
- Daily disposable soft lenses: Superior hygiene, reduced complications
- Extended wear silicone hydrogel: Enhanced oxygen permeability
- Multifocal designs: Address both hyperopia and presbyopia
- Annual investment: $300-$700, depending on lens type and replacement schedule
- Patient satisfaction: 85-92% report improved quality of life
Surgical Interventions
Corneal Refractive Surgery
LASIK (Laser-Assisted In Situ Keratomileusis) is the most widely performed refractive surgery worldwide. LASIK offers rapid visual recovery and high patient satisfaction for appropriate hyperopia cases.
Procedure specifications:
- Femtosecond laser flap creation (100-160 microns)
- Excimer laser corneal reshaping with peripheral steepening
- Optimal candidates: +1.00 to +4.00 D, stable refraction, adequate corneal thickness
- Success metrics: 85-95% achieve 20/40 or better vision
- Investment range: $1,500-$5,000 per eye (average $2,250)
- Recovery timeline: Visual improvement within 24-48 hours, full stabilization at 3-6 months
Important considerations for hyperopia:
- Higher regression rates compared to myopia correction
- Enhancement procedures are required in 15-20% of cases
- Age-related vision changes may affect long-term outcomes
PRK (Photorefractive Keratectomy) Surface ablation technique offering excellent long-term stability, particularly beneficial for patients with contraindications to LASIK.
Clinical advantages:
- No flap-related complications
- Suitable for thin corneas or irregular topography
- Cost range: $1,750-$4,000 per eye
- Recovery: Slower initial healing (5-7 days) but excellent outcomes
SMILE (Small Incision Lenticule Extraction) emerging minimally invasive technique showing promise for hyperopia correction, though it currently has limited FDA approval.
Lens-Based Surgical Options
Refractive Lens Exchange (RLE) is Optimal for patients over 50 or those with extreme hyperopia. RLE replaces the natural lens with an artificial intraocular lens.
Procedural benefits:
- Permanent correction with no regression
- Simultaneous presbyopia correction
- Prevention of future cataract development
- Investment: $3,000-$5,000 per eye
- Success rate: 95%+ achieve target refraction
IOL options:
- Monofocal lenses for distance correction
- Multifocal designs for presbyopia management
- Extended depth of focus (EDOF) lenses
- Light-adjustable lenses for post-surgical fine-tuning
Age-Specific Management Strategies
Children (Ages 3-18)
Early Detection is Critical
- Annual eye exams starting at age 3
- Watch for learning difficulties that may be vision-related
- Prompt treatment prevents amblyopia and strabismus
Treatment Approach
- Glasses are usually the first choice
- Full prescription correction is often necessary
- Contact lenses for older, responsible children
Adults (Ages 18-40)
Lifestyle Considerations
- Career demands (computer work, reading)
- Sports and recreation activities
- Aesthetic preferences
Treatment Flexibility
- Multiple correction options available
- Surgery candidacy assessment
- Balancing convenience with effectiveness
Older Adults (Ages 40+)
Addressing Multiple Vision Changes
- Hyperopia plus presbyopia management
- Considering cataract development
- Overall eye health monitoring
Comprehensive Solutions
- Multifocal lenses for glasses or contacts
- Surgical options addressing multiple issues
- Regular monitoring for age-related conditions
Living Successfully with Hyperopia: Practical Tips
Optimizing Your Environment
- Lighting: Use bright, even lighting for close work
- Computer use: Follow the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds)
- Reading setup: Position materials at a comfortable distance with good lighting
- Workplace ergonomics: Adjust monitor height and distance appropriately
Eye Health Maintenance
- Regular exams: Follow your eye doctor’s recommended schedule
- UV protection: Wear sunglasses with 100% UV protection
- Healthy lifestyle: Maintain good nutrition and stay hydrated
- Eye hygiene: Practice proper contact lens care if applicable
Prevention and Early Intervention
While you can’t prevent genetic hyperopia, early detection and proper management can prevent complications and optimize vision development.
For Parents:
- Schedule regular pediatric eye exams
- Watch for signs of vision problems
- Address concerns promptly with professionals
- Create vision-friendly learning environments
For Adults:
- Maintain regular eye exam schedules
- Protect eyes from injury and UV damage
- Manage underlying health conditions
- Stay informed about treatment advances
Clinical Evidence: Recent Research Advances
Landmark Studies Shaping Current Practice
Educational Impact Research (Hopkins et al., 2024). This pivotal study of school-aged children established that uncorrected hyperopia ≥+2.00 D significantly impairs academic performance and visual development. Key findings include:
- 40% reduction in reading comprehension scores
- Increased attention deficits during classroom activities
- Higher rates of behavioral issues are attributed to visual fatigue
- Strong correlation between hyperopia correction and improved academic outcomes
Beijing Hyperopia Reserve Study (2025). The largest pediatric hyperopia study to date, examining 2,109 preschool children, revealed critical insights into emmetropization patterns:
- 68% of children maintained adequate hyperopia reserve
- Strong correlation between parental myopia and reduced hyperopia reserve
- Geographic variations in hyperopia prevalence within single populations
- Early intervention recommendations for high-risk children
Global Prevalence Meta-Analysis (Updated 2025) Comprehensive analysis of 40 international studies confirmed:
- Significant ethnic variations in hyperopia prevalence
- Age-specific decline patterns from childhood to adolescence
- Regional differences correlating with genetic and environmental factors
- Implications for public health screening protocols
Special Considerations: When Hyperopia Requires Extra Attention
High Hyperopia (>+4.00 D)
- Increased risk of complications
- May require specialized treatment approaches
- Earlier intervention is often necessary
Hyperopia with Astigmatism
- More complex optical correction needed
- Specialized lens designs available
- Surgical planning requires additional considerations
Occupational Considerations
- Computer workers may need specialized lenses
- Pilots and drivers have specific vision requirements
- Healthcare workers need optimal near vision
Economic Considerations and Insurance Coverage
Investment Analysis for Hyperopia Treatment
Understanding the financial implications of hyperopia correction enables informed decision-making and optimal resource allocation.
Lifetime Cost-Benefit Analysis
- Conservative optical correction: $200-$600 initial investment, $100-$200 annual maintenance
- Contact lens programs: $300-$700 annually over 20+ years = $6,000-$14,000 lifetime cost
- Surgical intervention: $1,500-$10,000 one-time investment with potential 20+ year benefit
Insurance Coverage Landscape (2025)
Vision Insurance Benefits Most vision plans provide:
- Annual eyeglass allowance: $150-$400
- Contact lens alternative: $100-$300 annual allowance
- Exam coverage: Full coverage with modest copayments
Health Savings Account Eligibility: All hyperopia treatments qualify for HSA/FSA reimbursement:
- Pre-tax payment advantages
- 20-30% effective cost reduction based on tax bracket
- No “use it or lose it” restrictions for HSAs
Surgical Coverage Considerations
- Traditional insurance rarely covers elective refractive surgery
- Some employer plans offer partial reimbursement or payment programs
- Military and veteran benefits may include coverage
- Financing options are available through most surgical centers
Choosing the Right Eye Care Provider
What to Look for:
- Board certification in ophthalmology or optometry
- Experience with hyperopia treatment
- Access to modern diagnostic equipment
- Good communication and patient education
- Comprehensive approach to eye health
Questions to Ask:
- What treatment options are best for my situation?
- What are the risks and benefits of each approach?
- How often will I need follow-up care?
- What should I expect for recovery and results?
Future Outlook: Advances in Hyperopia Treatment
The field of vision correction continues to evolve rapidly:
Emerging Technologies:
- Advanced laser systems for more precise surgical outcomes
- Smart contact lenses with adjustable focus
- Gene therapy for inherited conditions
- Artificial intelligence for improved diagnostics
Research Directions:
- Better understanding of genetic factors
- Improved surgical techniques
- Novel pharmaceutical approaches
- Enhanced contact lens materials
Additional Resources & Scientific References
For healthcare professionals and patients seeking peer-reviewed evidence supporting hyperopia management decisions:
Primary Research Citations:
-
“Hyperopia in schoolchildren: Investigating the impact on vision and determining appropriate methods for screening” – Hopkins, R.C., et al. (2024)
Ophthalmic and Physiological Optics, Vol. 44, Issue 1
Landmark educational impact study demonstrating academic performance correlation with uncorrected hyperopia ≥+2.00 D in school-aged populations.
Access full research → -
“The hyperopia reserve in 3- to 6-year-old preschool children in North China: the Beijing hyperopia reserve research” – Pu, J., Fang, Y., et al. (2025)
BMC Ophthalmology, Volume 25, Article 175
Comprehensive epidemiological analysis of 2,109 preschool children establishing normative hyperopia reserve data and myopia risk stratification protocols.
View complete study → -
“Hyperopia: a meta-analysis of prevalence and a review of associated factors among school-aged children” – Castagno, V.D., et al. (2014, Updated Analysis 2025)
BMC Ophthalmology
Definitive systematic review and meta-analysis synthesizing global hyperopia prevalence data from 40 international studies, establishing evidence-based screening guidelines.
Read meta-analysis →
Professional Guidelines and Standards:
- American Academy of Ophthalmology Clinical Guidelines for Hyperopia Management
- International Council of Ophthalmology Refractive Surgery Guidelines
- American Optometric Association Pediatric Eye Examination Standards
This article reflects current evidence-based practice standards and incorporates the latest peer-reviewed research in hyperopia diagnosis and management..
View the meta-analysis →
These studies form the foundation of current evidence-based hyperopia management and provide the statistical data referenced throughout this article.
Conclusion: Taking Control of Your Vision
Hyperopia is a common, well-understood condition with excellent treatment options available today. Whether you’re experiencing symptoms for the first time or looking to optimize current treatment, working with a qualified eye care professional is your best path forward.
Remember: Early detection and proper treatment not only improve your vision but can also prevent complications and enhance your overall quality of life. Don’t let blurry near vision hold you back from enjoying reading, work, hobbies, and daily activities to their fullest.
Take the first step toward clearer vision by scheduling a comprehensive eye exam with a qualified provider in your area. Your eyes – and your quality of life – will thank you.
FAQs
-
Hyperopia (farsightedness) occurs when light focuses behind the retina instead of on it. This makes close objects blurry while distant vision may remain clear