Flashers and Floaters
Executive Summary: Eye floaters and flashes affect over 30% of adults, representing one of the most common visual complaints in ophthalmology. While typically benign manifestations of age-related vitreous changes, the acute onset of symptoms can herald sight-threatening conditions requiring immediate intervention. This evidence-based guide synthesizes current research, treatment protocols, and expert recommendations to help both patients and healthcare providers navigate this prevalent ocular phenomenon.
What Are Flashers and Floaters?
Understanding Eye Floaters
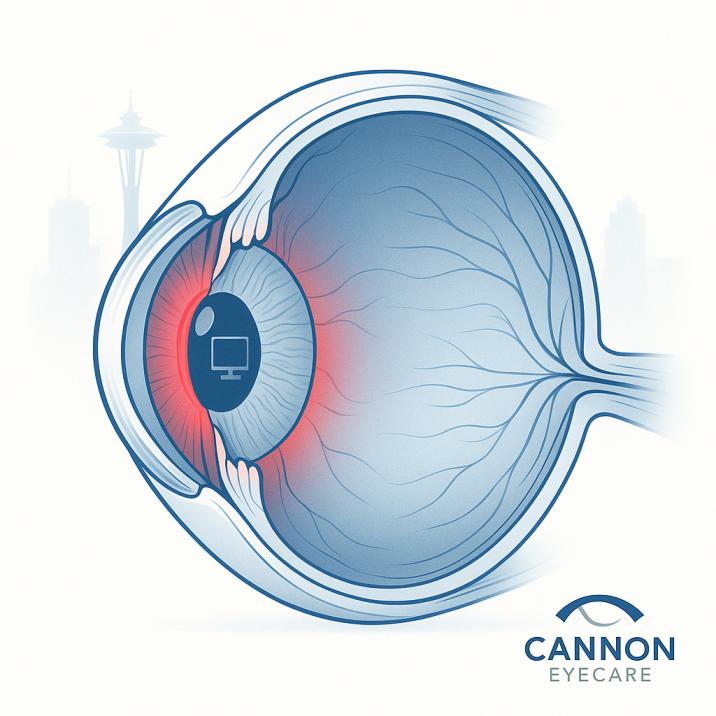
Eye floaters appear as small dark spots, threads, or cobweb-like shapes drifting across your vision. These aren’t actually floating in front of your eye—they’re shadows cast by tiny clumps of gel or cells inside your eye’s vitreous humor, the clear jelly-like substance filling most of your eyeball.
Common floater descriptions include:
- Small black dots or specks
- Thread-like strands
- Cobweb patterns
- Ring-shaped shadows (called Weiss rings)
- Translucent or blurry shapes
Understanding Eye Flashes
Eye flashes (medically called photopsias) are brief bursts of light appearing in your peripheral vision. They’re often described as:
- Lightning-like streaks
- Bright spots or sparks
- Shooting stars
- Arcs of light to the side
Flashes occur when your vitreous gel tugs or rubs against your retina—the light-sensitive tissue lining the back of your eye.
Understanding the Pathophysiology
Vitreous Anatomy and Age-Related Changes
The vitreous humor comprises 99% water and 1% collagen fibers, hyaluronic acid, and other proteins, maintaining the eye’s structural integrity while allowing light transmission to the retina. This gel-like substance undergoes predictable age-related modifications that directly contribute to floater development.
Primary pathophysiological processes include:
Vitreous Syneresis: Progressive liquefaction begins in the fourth decade, creating fluid-filled lacunae within the gel matrix. This process accelerates the breakdown of the collagen-hyaluronic acid complex that maintains vitreous transparency.
Posterior Vitreous Detachment (PVD): The most clinically significant change, occurring in approximately 50% of individuals by age 50 and 65% by age 65. The posterior vitreous cortex separates from the internal limiting membrane, often creating the classic “Weiss ring” floater from condensed vitreous around the optic disc.
Vitreous Condensation: Collagen fibrils aggregate into visible strands and opacities, casting shadows on the retina that patients perceive as floaters. The density and location of these condensations determine symptom severity.
Clinical Presentation and Symptomatology
Floater Characteristics
Primary floaters manifest as:
- Punctate opacities: Small, well-defined dark spots
- Linear strands: Thread-like shadows following eye movements
- Web-like configurations: Complex branching patterns
- Annular forms: Ring-shaped opacities (Weiss rings) from peripapillary vitreous detachment
Secondary floaters may present as:
- Dense, numerous opacities (vitreous hemorrhage)
- Inflammatory cells (uveitis-related)
- Pigmented particles (retinal tear debris)
Flash Phenomena (Photopsias)
Photopsias typically present as:
- Peripheral arc flashes: Brief streaks in temporal visual fields
- Central sparkles: Brief, bright spots in central vision
- Continuous flickering: Persistent light phenomena (concerning retinal traction)
Temporal patterns:
- Acute onset: Hours to days (high suspicion for PVD or retinal pathology)
- Chronic intermittent: Weeks to months (typical benign PVD evolution)
- Progressive increase: Concerning retinal complications
Common Symptoms and What They Mean
Typical Floater Descriptions
- Small black dots or specks
- Thread-like strands
- Cobweb patterns
- Ring-shaped shadows (Weiss rings)
- Blurry or translucent shapes
Normal Flash Characteristics
- Brief streaks of light in peripheral vision
- More noticeable in dark environments
- Intermittent occurrences over weeks or months
- Usually subsides as vitreous detachment completes
Risk Factors and Who’s Most Affected
Age-Related Risk
- 30% of people experience floaters occasionally, with research showing increased prevalence with age
- 50% of people develop posterior vitreous detachment (the main cause of floaters) by age 50
- 65% of people have posterior vitreous detachment by age 65
- Most common onset after age 50, though increasingly seen in younger adults with myopia
Additional Risk Factors
- Nearsightedness (myopia): Higher risk, especially with prescriptions over -3.00D
- Previous eye surgery: Particularly cataract surgery
- Eye trauma or injury
- Diabetes: Can cause bleeding that leads to floaters
- High blood pressure: May contribute to retinal changes
- Family history of retinal problems
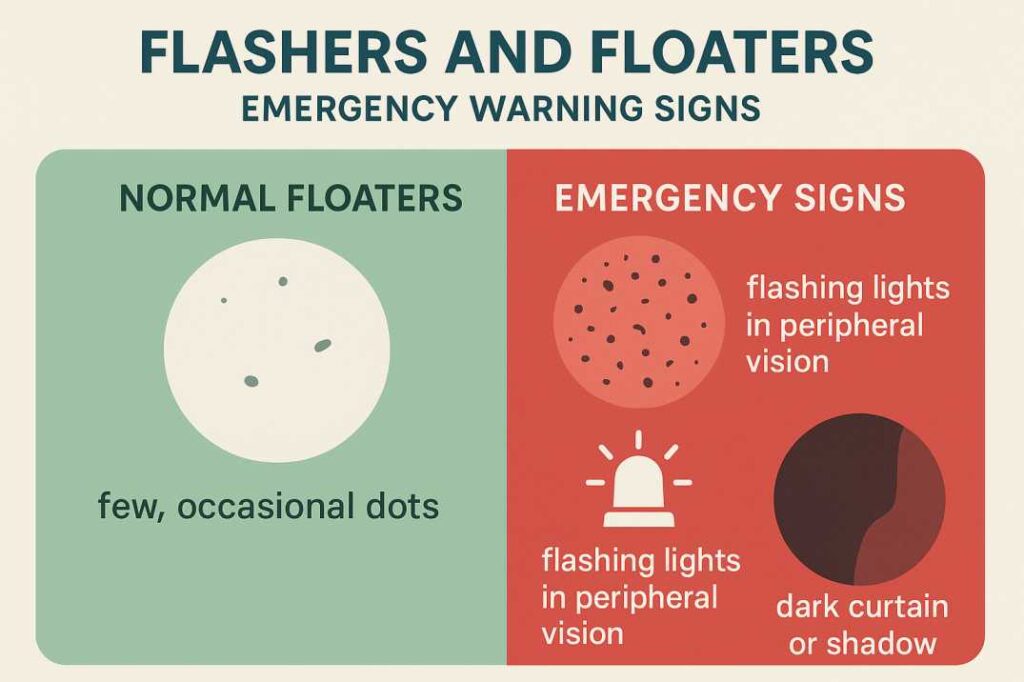
When Flashers and Floaters Become Concerning
Emergency Warning Signs – Seek Immediate Care
- Sudden shower of new floaters
- Persistent, frequent flashes curtain or a shadow moving across your vision
- Loss of peripheral vision
- Significant vision decrease
- New large floater accompanied by flashes
These symptoms may indicate serious conditions requiring urgent treatment:
Retinal Tear or Detachment
Occurs when vitreous pulling creates a hole in the retina or separates it from the underlying tissue. Without prompt treatment, this can lead to permanent vision loss.
Vitreous Hemorrhage
Bleeding into the vitreous cavity can cause a sudden increase in floaters and vision impairment.
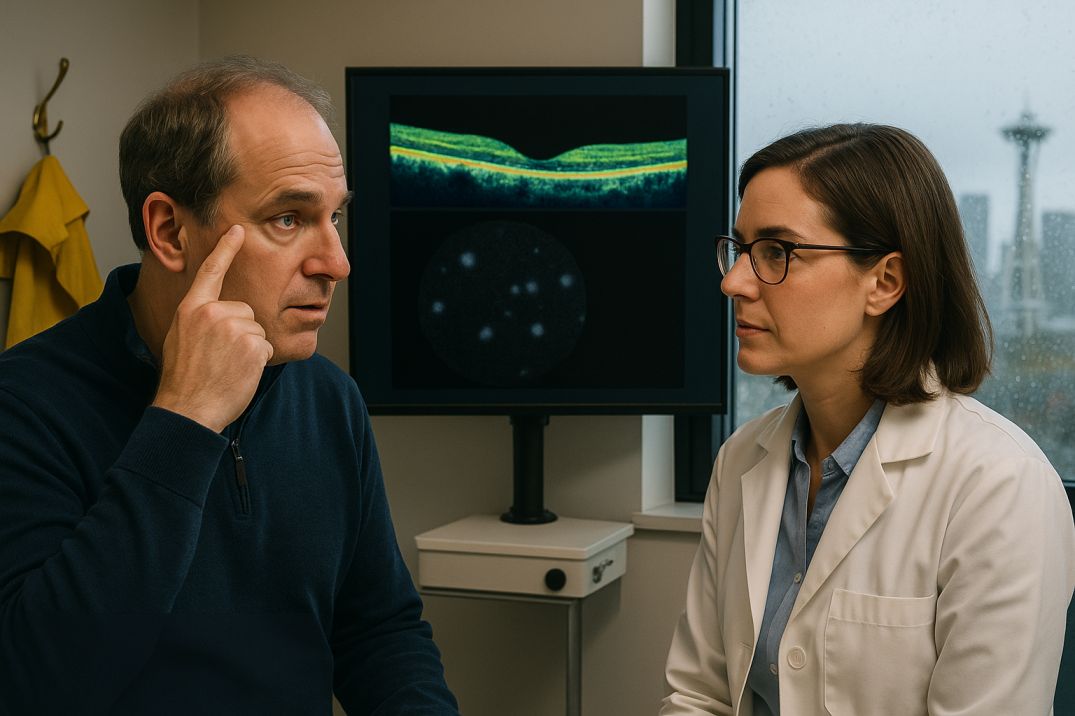
Diagnosis: What to Expect at Your Eye Exam
Comprehensive Evaluation
Your eye care provider will conduct:
- Detailed symptom history
- Visual acuity testing
- Pupil dilation for retinal examination
- Ophthalmoscopy to view the retina and vitreous
- Possible ultrasound imaging if the view is obscured
Questions Your Doctor May Ask
- When did symptoms start?
- Are floaters increasing in number?
- Do you see flashes of light?
- Any vision loss or shadowing?
- Previous eye surgeries or injuries?
- Family history of eye problems?
Treatment Options: From Watchful Waiting to Surgery
Conservative Management (Most Common)
For typical age-related floaters and flashes:
- Observation: Most floaters become less noticeable over time
- Lifestyle adjustments: Moving eyes up and down can temporarily shift bothersome floaters
- Regular monitoring: Follow-up exams to ensure no complications
Evidence-Based Treatment Paradigms
Conservative Management
The majority of patients (approximately 85%) with uncomplicated posterior vitreous detachment experience symptom resolution through neuroadaptation within 3-6 months. Conservative management remains the gold standard for most cases.
Clinical monitoring includes:
- Initial comprehensive examination with dilated funduscopy
- Follow-up at 4-6 weeks to assess for delayed complications
- Patient education regarding warning symptoms
- Reassurance regarding the benign nature of typical presentations
Laser Vitreolysis: Current Evidence
Mechanism: Nd: YAG laser photodisruption converts floater proteins into gas bubbles through plasma formation, theoretically reducing visual interference.
Clinical efficacy data:
- Shah & Heier (2017): Randomized controlled trial demonstrated 53% subjective improvement versus 0% in sham treatment (n=52, p<0.001)
- Success rates: Moderate improvement in 35.8% of patients, complete resolution in 2.5%
- Optimal candidates: Single, well-demarcated floaters >3mm from retina and >2mm from crystalline lens
Safety profile:
- Complication rate: 0.8-2.0% in recent large series
- Most frequent adverse events: Transient intraocular pressure elevation, symptomatic floater increase
- Serious complications: Retinal hemorrhage, cataract formation (rare)
Surgical Intervention: Pars Plana Vitrectomy
Indications:
- Vision-degrading myopia with objective visual function impairment
- Failed conservative management with a significant quality-of-life impact
- Patient preference after a comprehensive risk-benefit discussion
Surgical outcomes:
- Success rate: 90-95% subjective improvement
- Objective measures: Significant improvement in contrast sensitivity function
- Cost-effectiveness: $1,574 per quality-adjusted life year (highly cost-effective)
Contemporary techniques:
- Small-gauge instrumentation: 25G/27G systems reduce surgical trauma
- Core vitrectomy: Selective removal minimizes iatrogenic retinal breaks
- Advanced visualization: 3D surgical systems improve safety profiles
Treatment for Serious Complications
- Retinal tears: Laser photocoagulation or cryotherapy
- Retinal detachment: Various surgical approaches, including scleral buckling or vitrectomy
- Vitreous hemorrhage: May require surgical intervention depending on the cause
Living with Flashers and Floaters: Practical Management Tips
Coping Strategies
- Adjust lighting: Reduce contrast between floaters and background
- Eye movement: Gentle eye movements can shift floaters out of direct vision
- Acceptance and adaptation: Most people’s brains learn to ignore chronic floaters
- Regular check-ups: Maintain annual eye exams, more frequent if symptoms change
Lifestyle Considerations
- Wear protective eyewear during sports or activities with eye injury risk
- Manage underlying conditions like diabetes and hypertension
- Avoid excessive eye rubbing
- Stay informed about warning signs requiring immediate care
Recent Research and Innovations
Breakthrough Studies in 2024-2025
Vision-Degrading Myodesopsia (VDM): Research published in 2024 identified that floaters can cause measurable vision degradation, with contrast sensitivity declining by up to 91% in severe cases, leading to new diagnostic criteria and treatment approaches.
Early Laser Intervention Study: A 2024 randomized clinical trial is evaluating the efficacy and safety of early YAG laser vitreolysis for symptomatic floaters, potentially changing treatment timing recommendations.
Functional Eye Dressing Research: Innovative 2022 research demonstrated recovery rates of 70% for mild floaters using oxygen and hydrogen therapy through specialized eye dressings, though this requires further validation.
Emerging Treatment Technologies
- Improved laser systems with better targeting capabilities
- Nanoparticle-based therapies showing promise in preclinical studies
- Enhanced surgical techniques using smaller-gauge instruments
- Objective measurement tools for better treatment planning
Prevention: Can You Avoid Flashers and Floaters?
While age-related changes are inevitable, you can potentially reduce risk through:
Health Management
- Control diabetes and blood pressure
- Regular eye exams for early detection
- Protective eyewear during high-risk activities
- A healthy lifestyle supports overall eye health
Clinical Decision-Making Framework
Risk Stratification Protocol
Low-risk presentations:
- Gradual onset over weeks to months
- Stable symptoms without progression
- No associated photopsias or visual field defects
- Clear media on examination
Intermediate-risk presentations:
- Recent symptom onset (days to weeks)
- Associated intermittent photopsias
- High myopia or previous intraocular surgery
- Requires urgent but not emergent evaluation
High-risk presentations requiring immediate assessment:
- Acute onset with “shower” of floaters
- Persistent or increasing photopsias
- Associated visual field defects or “curtain” phenomenon
- Previous retinal pathology or family history of retinal detachment
Contemporary Management Algorithms
Initial assessment protocol:
- Comprehensive history: Timing, associated symptoms, risk factors
- Visual function testing: Best-corrected acuity, confrontation fields
- Dilated examination: Complete peripheral retinal evaluation
- Documentation: Detailed findings for medicolegal purposes
Follow-up scheduling:
- Routine floaters: Annual examination unless symptoms change
- Recent PVD: 4-6 week follow-up, then as needed
- High-risk features: Immediate ophthalmologic consultation
Special Considerations for Different Age Groups
Young Adults (20-40)
- Floaters are increasingly common due to rising myopia rates (up to 80-90% in some regions)
- Often more distressing due to the unexpected nature and longer time living with symptoms
- May be candidates for earlier intervention with laser treatment
- Important to rule out underlying conditions like high myopia complications
Middle Age (40-65)
- Most common time for initial floater development
- Regular eye exams become more crucial
- Higher likelihood of posterior vitreous detachment
- Balance between observation and intervention
Seniors (65+)
- Highest prevalence of floaters and flashes
- Greater risk of complications
- Need for more frequent monitoring
- Consideration of overall health in treatment decisions
The Psychological Impact: Addressing Quality of Life
Understanding the Emotional Response
Research shows that bothersome floaters can cause:
- Depression and anxiety
- Reduced quality of life
- Difficulty with daily activities
- Social withdrawal
Studies indicate patients would trade one year of life from each remaining decade to be free of severe floaters, highlighting the significant psychological impact.
Support and Resources
- Patient education about the benign nature of most floaters
- Support groups and online communities
- Mental health resources when symptoms cause distress
- Realistic expectations about treatment outcomes
Choosing the Right Eye Care Provider
When dealing with flashers and floaters, consider:
Types of Specialists
- Optometrists: Primary eye care and basic evaluations
- Ophthalmologists: Medical and surgical eye care
- Retina specialists: Advanced training in vitreoretinal conditions
Questions to Ask Your Provider
- Experience with floater treatments
- When to consider intervention
- Surgical expertise and outcomes
- Emergency contact procedures
- Follow-up care protocols
Conclusion: Taking Control of Your Eye Health
Flashers and floaters are common experiences that affect millions of people worldwide. While the vast majority are harmless results of natural aging, understanding when to seek immediate care can prevent serious vision loss. The key is education, regular monitoring, and prompt attention to warning signs.
Expert Commentary and Future Directions
Flashers and floaters represent a fascinating intersection of normal aging, pathological processes, and evolving treatment paradigms. The recent recognition of vision-degrading myodesopsia as a legitimate clinical entity has transformed our approach from dismissive reassurance to evidence-based intervention.
Key clinical pearls:
- Neuroadaptation remains the most successful “treatment” for the majority of patients
- Objective visual function testing should guide intervention decisions
- Patient education and expectation management are crucial for optimal outcomes
- Technology continues to improve safety profiles for both laser and surgical interventions
Future research priorities:
- Biomarkers for predicting PVD complications
- Pharmacological prevention of pathological vitreous changes
- Artificial intelligence integration for risk stratification
- Long-term outcomes data for emerging treatment modalities
The field continues to evolve rapidly, with promising developments in both diagnostic capabilities and therapeutic options. As our understanding of vitreous biochemistry and patient-reported outcomes improves, we anticipate more personalized, evidence-based approaches to this common yet challenging clinical scenario.
Additional Resources and Expert Citations
For those seeking more detailed medical information and current research on flashers and floaters, these authoritative sources provide comprehensive, evidence-based insights:
1. American Academy of Ophthalmology – Floaters and Flashes Guide
Link: https://www.aao.org/eye-health/diseases/what-are-floaters-flashes
Why It’s Valuable: The nation’s leading professional organization of ophthalmologists provides patient-friendly explanations backed by clinical expertise. This resource offers the most current professional guidelines on when to seek immediate care and what warning signs require urgent attention.
2. JAMA Ophthalmology – Randomized Clinical Trial on Laser Treatment
Citation: Shah, C.P., Heier, J.S. (2017). “YAG laser vitreolysis vs sham YAG vitreolysis for symptomatic vitreous floaters: a randomized clinical trial.” JAMA Ophthalmology, 135(9), 918-923.
Why It’s Important: This landmark study provides the gold standard evidence for laser treatment effectiveness, showing 53% of patients experienced significant improvement. It’s the most rigorous scientific evaluation of laser vitreolysis available.
3. Cleveland Clinic – Comprehensive Posterior Vitreous Detachment Information
Link: https://my.clevelandclinic.org/health/diseases/14413-posterior-vitreous-detachment
Why It’s Essential: The Cleveland Clinic’s detailed explanation of posterior vitreous detachment helps readers understand the most common cause of flashers and floaters. Their content includes expert-reviewed information on symptoms, risk factors, and when complications might occur.
Conclusion
Flashers and floaters exemplify the complexity of modern ophthalmology, where common symptoms can range from benign age-related changes to vision-threatening emergencies. This comprehensive review synthesizes current evidence to provide healthcare professionals and patients with the knowledge necessary for optimal clinical decision-making.
The evolution from observational management to evidence-based interventions reflects our improved understanding of visual quality and patient-centered care. As diagnostic techniques become more sophisticated and treatment options expand, the future promises even better outcomes for patients affected by these prevalent visual phenomena.
Early recognition of high-risk presentations, appropriate use of emerging technologies, and emphasis on patient education remain the cornerstones of excellent clinical care in this domain. The continued collaboration between researchers, clinicians, and patients will undoubtedly yield further advances in our understanding and management of flashers and floaters.
Always consult with a qualified eye care professional for proper diagnosis and treatment recommendations. This information is for educational purposes and should not replace professional medical advice.
FAQs
-
Eye floaters are small specks, dots, or cobweb-like shapes that drift in your field of vision. They’re caused by tiny cell clusters or protein particles floating in the vitreous gel inside your eye.