If you’ve noticed small dark spots drifting across your vision or sudden flashes of light, you’re experiencing two of the most common eye symptoms that bring people to Seattle eye doctors. While floaters and flashes are often harmless age-related changes, they can sometimes signal serious conditions requiring immediate medical attention. Understanding when these visual disturbances warrant urgent care versus routine monitoring could save your sight.
Bottom Line Up Front: New, sudden floaters, especially when accompanied by flashes of light, require same-day evaluation by an eye care professional. Don’t wait if you experience a “shower” of new floaters, persistent flashing lights, or any loss of peripheral vision.
Understanding Eye Floaters and Flashes – The Basics
What Are Eye Floaters?
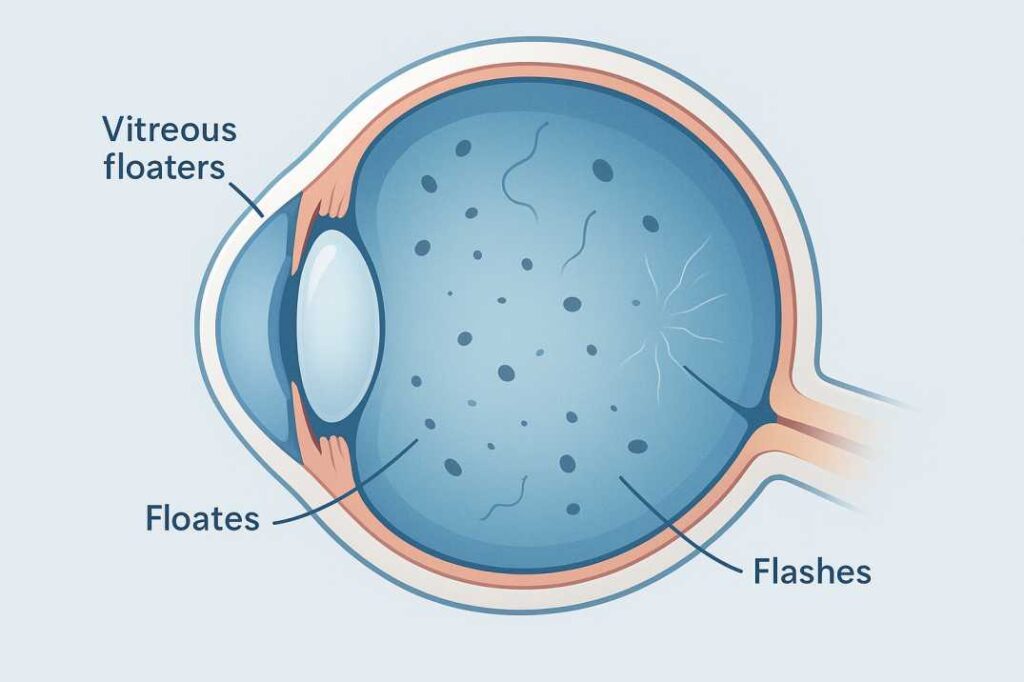
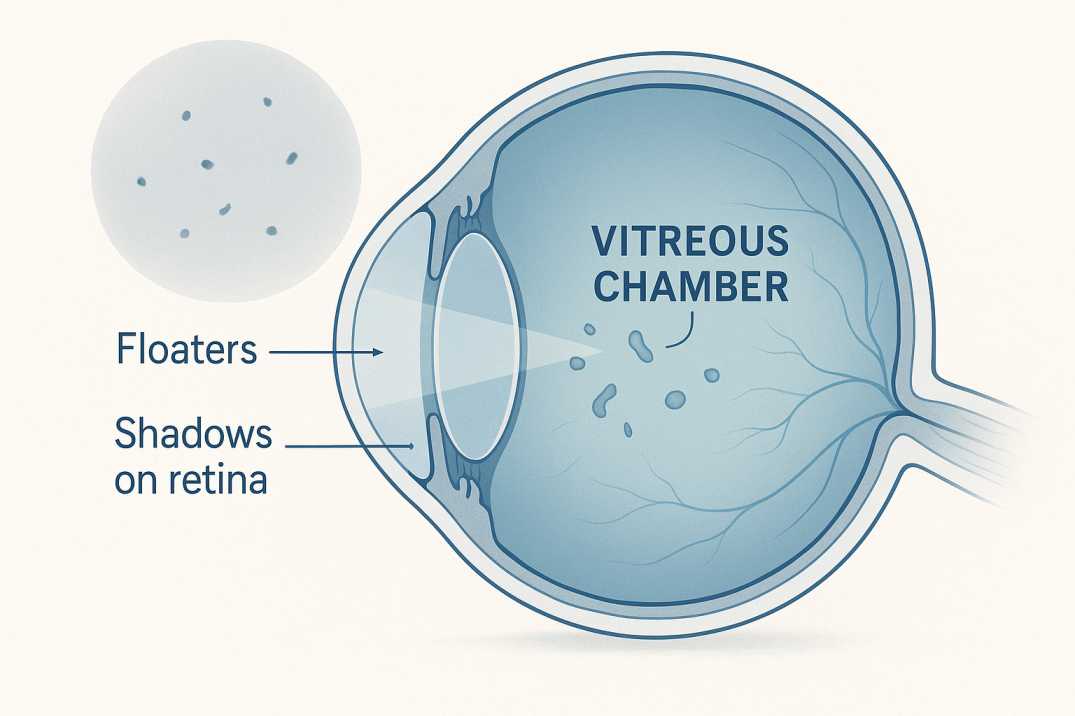
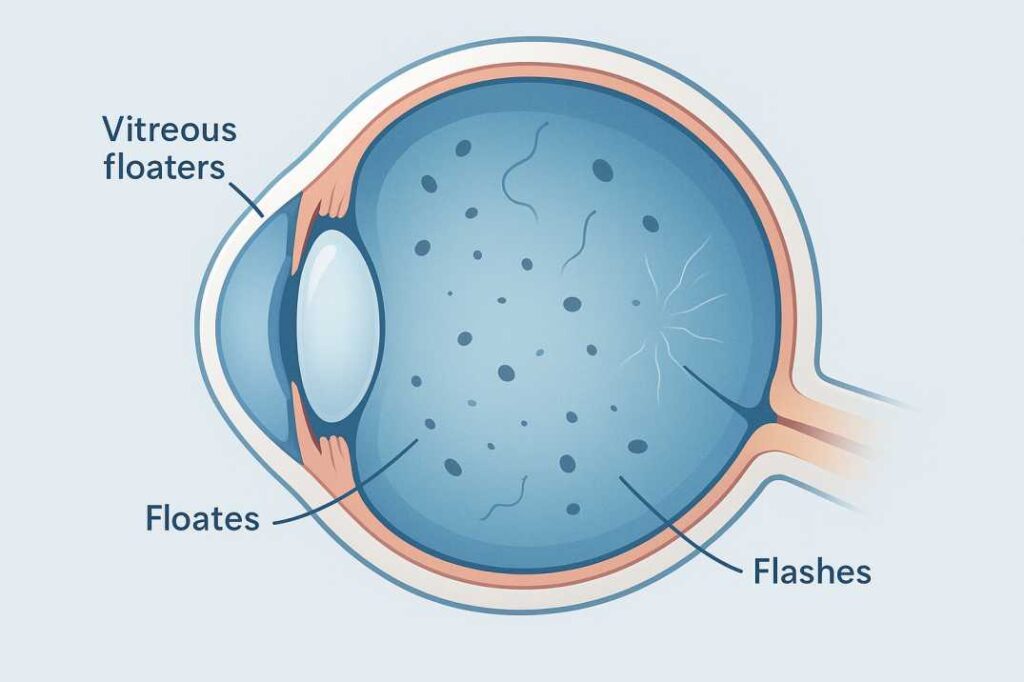
Floaters look like specks, dots, circles, lines, or cobwebs in your field of vision. While they seem to be in front of your eye, they are floating inside. These visual phenomena occur when tiny pieces of the eye’s vitreous break loose and cast shadows on your retina.
The vitreous humor is a clear, gel-like substance that fills approximately 80% of your eye’s interior. As we age, the natural gel-like fluid in the vitreous starts to contract, creating tiny clumps or strands that appear as moving shadows in our vision.
Common descriptions of floaters include:
- Squiggly lines or threads
- Dark spots or specks
- Cobweb-like strands
- Small shadowy shapes
- Ring-shaped formations (called Weiss rings)
What Are Eye Flashes?
Flashes in the form of bright spots, streaks of lightning, or shooting stars in the corner of your eye can indicate a serious medical condition when they occur suddenly or repeatedly. When the vitreous gel inside your eye rubs or pulls on the retina, you may see what looks like flashing lights or lightning streaks.
These light phenomena typically appear as:
- Brief lightning bolt-like streaks
- Camera flash-type bursts
- Flickering lights in peripheral vision
- Bright spots or sparks
How Common Are These Symptoms?
About one-quarter of people have some vitreous shrinkage with floaters by their 60s; that rises to about two-thirds of 80-year-olds. PVD is a very common, age-related condition. It’s estimated that 66% of people between the ages of 66 and 86 will develop the condition.
However, for Seattle residents aged 28-55 who are experiencing these symptoms for the first time, the sudden onset requires professional evaluation to rule out serious complications.
Emergency Warning Signs – When to Seek Immediate Care
Red Flag Symptoms Requiring Urgent Attention
Seek immediate eye care if you experience:
One new, large floater or “showers” of floaters appear suddenly. You see sudden flashes of light, especially if these flashes are persistent.
You notice other symptoms, such as the loss of side vision, or if it looks as if a shade or curtain is being drawn over your field of vision
Additional emergency indicators:
- Sudden increase in the number or size of floaters
- Flashes of light that persist or increase in frequency
- A dark “curtain” or shadow moving across your field of vision
- Sudden vision loss or significant vision changes
- Eye pain accompanying new floaters or flashes
For patients with an acute onset of floaters and/or flashes who are self-referred or referred to an ophthalmologist, the prevalence of retinal tear is 14%. This statistic from recent research underscores why prompt evaluation is crucial.
Seattle Emergency Eye Care Options
For urgent eye care needs in Seattle, you have several options:
Immediate Care Locations:
- University of Washington Medical Center Eye Institute
- Seattle Children’s Hospital (for pediatric cases)
- Virginia Mason Medical Center Ophthalmology
- Swedish Medical Center Eye Emergency Services
After-Hours Options: If your regular eye doctor isn’t available, most emergency departments can provide initial assessment and contact on-call ophthalmologists when necessary.
What to Expect During an Emergency Visit
Your eye doctor can check your eyes with a dilated eye exam. Your doctor will give you some eye drops to dilate (widen) your pupil and then look at your retina at the back of your eye.
The emergency evaluation typically includes:
- Visual acuity testing
- Pupil dilation for retinal examination
- Slit lamp examination of the anterior eye
- Indirect ophthalmoscopy to examine the peripheral retina
- Assessment for vitreous hemorrhage or pigment cells
Normal vs Concerning Floaters and Flashes
Age-Related Changes vs Serious Conditions
Normal Floaters:
- Few in number and stable over time
- More noticeable against bright backgrounds
- Move when you move your eyes
- Don’t significantly impair vision
- May be present for years without change
Concerning Floaters: If you experience an acute (sudden) onset of floaters and flashes, you should see an eye care provider
- Sudden appearance of many new floaters
- Dramatically increased size or density
- Accompanied by flashing lights
- Associated with vision loss or visual field defects
Risk Factors to Consider
Certain factors increase your likelihood of developing serious complications:
High-Risk Categories:
- Very nearsighted people (high myopes) are at greater risk of developing floaters earlier in life and are also at a greater risk of a retinal tear or detachment
- History of eye surgery (especially cataract surgery)
- Previous eye trauma or injury
- Family history of retinal detachment
- Diabetes or other systemic conditions affecting blood vessels
Recent studies using smartphone-based surveys found that 76% of people report seeing floaters, with 33% reporting that floaters caused noticeable impairment in vision. Research shows that while floaters increase with age, the effect becomes more pronounced after age 50.
When Routine Monitoring is Appropriate
Chronic floaters usually aren’t something you need to be concerned about, but it’s a good idea to have your eyes regularly checked to make sure there aren’t any other serious eye issues.
Schedule routine follow-up if:
- Floaters are stable and not increasing
- No associated flashing lights
- Vision remains clear and unchanged
- Symptoms develop gradually over months or years
Common Causes and Medical Conditions
Posterior Vitreous Detachment (PVD)
Posterior Vitreous Detachment (PVD) is a natural change that occurs during adulthood, when the vitreous gel that fills the eye separates from the retina. This is the most common cause of new floaters and flashes.
PVD Characteristics:
- Most patients experience PVD after age 60, once in each eye
- Usually, a benign, self-limiting process
- About 85% of patients who experience PVD never develop complications, and in most cases, the flashes and floaters subside within 3 months.hs
- May cause a large ring-shaped floater (Weiss ring)
Retinal Tears and Detachment
A recent study published in Ophthalmology showed that, among people who experienced the sudden symptom of eye floaters and/or flashes of light, 39.7 percent had a posterior vitreous detachment and 8.9 percent had a torn retina.
Warning Signs of Retinal Complications: A warning sign of a retinal tear is repeated flashes that could occur within seconds or hours of each other. Other signs include a sudden increase in floaters, a curtain in front of the eye, a loss of peripheral vision, or a narrowing of the visual field.
Why Immediate Treatment Matters: If left untreated, a retinal detachment may lead to permanent loss of vision. Early detection and treatment can often preserve vision through laser therapy, cryotherapy, or surgical repair.
Other Contributing Factors
Additional causes of floaters and flashes include:
Medical Conditions:
- Diabetic retinopathy
- Vitreous hemorrhage
- Uveitis (eye inflammation)
- Migraine with aura
- High blood pressure effects on retinal vessels
Recent Research Findings: Vitreous opacification results from fibrous liquefaction, a progressive process that begins in youth and advances more rapidly in myopic eyes, leading to myopic vitreopathy. This 2023 research highlights why younger, nearsighted individuals may experience floaters earlier than expected.
Diagnostic Process and What to Expect
Your Seattle eye doctor will perform several key assessments:
History Taking:
- Duration and onset of symptoms
- Associated visual changes
- Previous eye problems or surgeries
- Family history of eye disease
- Current medications and health conditions
Physical Examination: A slit lamp exam is needed to examine the anterior vitreous for pigmented cells (Shaffer sign), and indirect ophthalmoscopy with scleral indentation can rule out a retinal tear or break.
Advanced Imaging and Testing
When indicated, additional testing may include:
Optical Coherence Tomography (OCT):
- Detailed cross-sectional images of retinal layers
- Can detect subtle retinal changes
- Non-invasive and painless
Ultrasound Examination:
- Used the en view of the retina is obscured
- Helpful in detecting retinal detachment
- Can assess vitreous hemorrhage
Fluorescein Angiography:
- Evaluates retinal blood flow
- Identifies vascular abnormalities
- Used in complex cases
Questions Your Seattle Eye Doctor Will Ask
Be prepared to discuss:
- Exact timing of symptom onset
- Changes in symptom severity or frequency
- Associated vision loss or visual field defects
- Recent trauma or eye procedures
- Family history of retinal problems
- Current medications, especially blood thinners
Treatment Options and Management
Conservative Management Approaches
For benign floaters from PVD:
Observation and Monitoring: PVD is non-sight-threatening, and the symptoms subside in the vast majority of patients. Most patients no longer notice flashes after 3 months, and floaters tend to improve.
Lifestyle Adaptations:
- Regular eye exams to monitor changes
- Patient education about warning signs
- Activity modifications if symptoms are bothersome
- Understanding that brain adaptation occurs over time
Surgical Interventions When Necessary
For Retinal Tears: Pinpoints of laser light can be used to fuse the retina to the back wall of the eye. Extreme cold, a procedure called cryopexy, does much the same thing.
For Severe Floaters (Vitrectomy): PPV is a surgical procedure utilized to remove vitreous gel. Although the procedure has been performed for over forty years, the instrumentation has improved significantly over the past two decades.
Recent 2024 research shows patients report subjective improvement in vision and performance of daily activities, leading to an enhanced quality of life following vitrectomy for symptomatic floaters.
Long-term Monitoring and Care
Follow-up Schedule: Patients with uncomplicated posterior vitreous detachment should be re-examined by an ophthalmologist at six weeks, as 3.4% will have a new retinal tear.
Ongoing Assessment:
- Annual dilated eye exams
- Prompt evaluation of new symptoms
- Coordination with retinal specialists when needed
- Patient education about self-monitoring
Finding the Right Seattle Eye Care Provider
Choosing Between Optometrists and Ophthalmologists
Optometrists can:
- Perform comprehensive eye exams
- Detect and monitor floaters and flashes
- Provide initial assessment and education
- Refer to specialists when necessary
Ophthalmologists offer:
- Surgical intervention capabilities
- Advanced diagnostic equipment
- Subspecialty expertise (retinal specialists)
- Management of complex eye diseases
Specialist Referrals and Retina Experts
For complex cases, you may need a retinal specialist who can provide:
- Advanced vitreoretinal surgery
- Expertise in posterior segment diseases
- Latest treatment technologies
- Coordination with other subspecialists
Seattle Retinal Specialists to consider:
- Seattle Retinal Consultants
- Northwest Eye Surgeons (Retina Division)
- University of Washington Retina Service
- Virginia Mason Retina Associates
Insurance and Accessibility Considerations
Coverage Information:
- Most insurance plans cover medically necessary eye examinations
- Emergency evaluations are typically covered under medical benefits
- Surgical procedures require prior authorization in most cases
- Vision insurance may have different coverage rules
Seattle-Specific Resources:
- Community health centers offering sliding scale fees
- University of Washington resident clinics
- County hospital emergency services
- Transportation resources for elderly or disabled patients
Recent Scientific Evidence Supporting Early Intervention
Three recent studies underscore the importance of prompt evaluation:
Study 1: Meta-Analysis of Retinal Tear Risk (2024)
A systematic review found that for patients with an acute onset of floaters and/or flashes, the prevalence of retinal tear is 14%. Subjective visual reduction is the most important symptom associated with retinal tear (likelihood ratio 5.0). This research emphasizes why Seattle residents shouldn’t delay seeking care when experiencing new symptoms.
Study 2: Vision Degrading Myodesopsia Research (2024)
This study corroborates previous findings of an association between vitreous degeneration and PVD with degradation in contrast sensitivity. The research highlights that floaters can significantly impact quality of life and visual function, validating patient concerns about these symptoms.
Study 3: Advanced Vitrectomy Outcomes (2024)
Studies have determined that patients perceive floaters as comparable to age-related macular degeneration and worse than glaucoma, diabetic retinopathy, mild angina, mild stroke, colon cancer, and asymptomatic AIDS. This finding emphasizes that dismissing floaters as “just part of aging” doesn’t address the real impact on patients’ lives.
Prevention and Risk Reduction
While many causes of floaters and flashes are age-related and unavoidable, certain strategies may help:
General Eye Health:
- Regular comprehensive eye exams
- Management of diabetes and blood pressure
- Protection from eye trauma
- Smoking cessation
- UV protection
When to Increase Monitoring:
- After age 50
- If you’re highly nearsighted
- Following eye surgery
- With a family history of retinal problems
References and Medical Resources
Key Clinical Studies and Evidence Sources
1. Hollands H, Johnson D, Brox AC, et al. Acute-onset floaters and flashes: Is this patient at risk for retinal detachment? JAMA. 2009;302(20):2243-2249. This comprehensive meta-analysis of 17 studies established the 14% prevalence rate of retinal tears among patients presenting with acute floaters and flashes. The study identified key risk factors, including subjective visual reduction (likelihood ratio 5.0) and vitreous hemorrhage presence (likelihood ratio 10.0), forming the evidence base for emergency evaluation protocols referenced throughout this article.
[PubMed Link: https://pubmed.ncbi.nlm.nih.gov/19934426/]
2. Demographics and Seasonality of Retinal Detachment, Retinal Breaks, and Posterior Vitreous Detachment from the Intelligent Research in Sight Registry Ophthalmology Retina. 2022;6(10):1016-1023. This large-scale database analysis of the IRIS Registry provided current epidemiological data on posterior vitreous detachment prevalence by age groups (24% at ages 50-59, increasing to 87% by age 80+) and confirmed that retinal breaks occur in 8-16% of patients with acute symptomatic PVD, with 30-50% progression to retinal detachment if untreated.
[PMC Link: https://pmc.ncbi.nlm.nih.gov/articles/PMC9559074/]
3. Gishti O, van den Nieuwenhof R, Verhoekx J, van Overdam K. Symptoms related to posterior vitreous detachment and the risk of developing retinal tears: a systematic review. Acta Ophthalmologica. 2019;97(4):347-352. This systematic review analyzed the relationship between specific symptoms and retinal tear development, establishing that 3.4% of patients with uncomplicated PVD develop retinal tears within 6 weeks. The study provided evidence-based follow-up protocols and risk stratification criteria used in the clinical decision-making sections of this article.
[PubMed Link: https://pubmed.ncbi.nlm.nih.gov/30632695/]
Additional Professional Resources
Clinical Decision-Making: Emergency versus Routine Care
Immediate ophthalmologic consultation indicated for:
- Acute-onset floaters or flashes, particularly with concurrent symptoms
- Sudden increase in pre-existing floater burden
- Visual field deficits or curtain-like phenomena
- Acute vision loss or significant acuity reduction
- Persistent photopsia with associated symptoms
Routine ophthalmologic care is appropriate for:
- Stable, chronic floaters without progression
- Gradual symptom onset over extended periods
- Isolated symptoms without vision changes
- Asymptomatic patients with a family history but no active symptoms
Evidence-Based Recommendations for Seattle Residents: Current evidence strongly supports immediate evaluation for acute-onset symptoms. Delayed presentation may compromise treatment efficacy and visual outcomes. Seattle’s comprehensive ophthalmologic infrastructure ensures accessible emergency care, eliminating barriers to timely evaluation.
Early detection of retinal pathology enables vision-preserving interventions, while appropriate reassurance regarding benign changes provides valuable patient education and peace of mind. When clinical uncertainty exists, professional evaluation remains the most prudent approach.
Cannon EyeCare at Market Optical provides comprehensive ophthalmologic evaluation for floaters and flashes, combining clinical expertise with personalized patient care. Our University Village and Pike Place Market locations offer state-of-the-art diagnostic capabilities, enabling precise assessment of vitreoretinal pathology. Our experienced optometrists utilize advanced imaging technologies to differentiate benign from pathological presentations, providing clear guidance regarding emergency referral versus routine monitoring protocols.
We maintain collaborative relationships with Seattle’s leading retinal specialists, ensuring seamless transitions for patients requiring subspecialty care. Our comprehensive approach addresses both immediate clinical concerns and long-term ocular health maintenance. Schedule your consultation to discuss any concerns regarding new floaters, persistent photopsia, or other visual symptoms. We accept major insurance plans and offer convenient online scheduling for Seattle-area residents.