Thermal Therapies For Dry Eye and MGD

Have you been suffering from Dry eye or MGD? Thermal therapies for dry eye and MGD could be the solution you’re looking for. In this article you can get all the information you need about Dry Eye and Meibomian Gland Dysfunction (MGD) and how you can treat them with Thermal Therapies for dry eye.
What Is MGD?
Meibomian Gland Dysfunction (MGD) is a condition characterized by the dysfunction or blockage of the meibomian glands, which are located in the eyelids. These glands produce the oily component of the tear film (meibum) that coats the ocular surface, helps lubricate the eyes and prevent tears from evaporating too quickly.
What Is Dry Eye?
Dry eye, also known as dry eye syndrome, dry eye disease, ocular surface disease or keratoconjunctivitis sicca, is a common condition that occurs when there is a lack of sufficient moisture or lubrication on the surface of the eyes. It can result from either decreased tear production or increased tear evaporation. Recent studies have shown that about half of Americans will experience dry eye as they age.
Is MGD The Same Thing As Dry Eye?
Meibomian Gland Dysfunction (MGD) and dry eye are often grouped together because they exhibit similar symptoms, including irritation, intermittent blur, itching, and/or burning. However, the underlying causes differ, and in fact there are 2 main types of dry eye: aqueous deficient (when there’s a lack of liquid tears production) and evaporative dry eye, which involves MGD.
Evaporative dry eye is what you’ve got if the tears you do have are poor quality. Having poor-quality tears means that your tears are unstable and evaporate too quickly. This is what our eye doctors are checking when they have you try not to blink at the bright blue light for a full 10 seconds. If the eye doctor observes a Tear Break-Up Time (TBUT) of less than 10 seconds, that is a sign of evaporative dry eye. Recent studies have shown that 86% of patients symptomatic for dryness have the evaporative type. So if your eyes are dry, the odds are good that you have underlying MGD. It is noteworthy that you can have both the aqueous and evaporative forms of dry eye.
Dr. Mark Cannon now has advanced imaging capability at our Pike Place office. He routinely captures infra-red images of the meibomian glands for our dry eye patients with our new advanced Firefly slit lamp microscope.

Evaporative & Aqueous Dry Eye
Recognizing the distinction between evaporative and aqueous dry eye is crucial when selecting an appropriate treatment.
In terms of tear composition, the tear film consists of three layers. The oily layer, produced by the meibomian glands, prevents rapid evaporation of tears and maintains a smooth surface. The watery layer, generated by the lacrimal glands, constitutes the actual tears. Lastly, the mucus layer, created by the conjunctiva, aids in spreading the tears evenly.
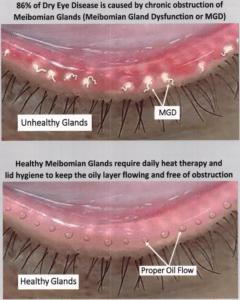
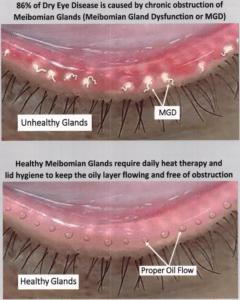
In cases of MGD, the meibomian glands fail to secrete sufficient healthy oils due to clogging of the exit pore or the oils being too thick – like butter or crisco. If the miebomian glands are not releasing oils frequently due to poor blinking or chronic clogging, the glands can atrophy – See image above. Often times the oily secretions will flow if forced, but are too thick and poor quality to move without intervention.
Consequently, tears evaporate too quickly (a fast TBUT), leading to dryness in the eyes. On the other hand, aqueous dry eye occurs when the lacrimal glands are unable to produce an adequate volume of tears. This may be caused by factors such as gland damage, medication usage, or medical conditions like Sjogrens Disease diabetes and lupus. Additionally, liquid tear production can be greatly effected by hydration levels and naturally slows down with age. The vast majority of Dr. Mark Cannon’s dry eye patients start out chronically dehydrated when they first seek him out for treatment.
Both MGD and aqueous dry eye can be treated, although our therapeutic approaches differ.
Recent investigations into dry eye disease have found that 86% of dry eye patients have Meibomian Gland Dysfunction (MGD). There are a number of things that cause MGD, such as aging, blepharitis, and lots of screen time. Another big factor is how thoroughly you blink; more on that later in this post.
Eye doctors have become increasingly aware of the importance of healthy, functional meibomian glands in recent years. The oils they release into the tears (creating the ‘lipid layer’) from the edge of your lid are a key component to healthy tears. If the glands are clogged or blocked, your tear quality will suffer as a result. This causes quick evaporation of the watery portion of your tears, with a resulting intermittent blur and discomfort or burning.
Your optometrist or ophthalmologist can determine how many glands are currently obstructed by pressing gently on your lids in a few different spots. Many offices (including Cannon EyeCare at Pike Place’s Market Optical) have specialized infra-red cameras that can image these meibomian glands. Often getting a baseline image is useful to track for future changes. This type of imaging is inexpensive and we can often bill the cost to insurance. We like to capture imaging of the meibomian glands annually to watch for change.
What To Consider When using Thermal Therapies for dry eye and MGD?
When addressing MGD, it’s important to recognize that two factors require attention: addressing obstruction and inflammation of the gland. The gland obstruction issue involves the physical blockage of the exit port for the gland. Obstructions can be removed by treating an overgrowth of bacteria on the lids known as blepharitis, eliminating an infestation of the lash follicles by Demodex mites, and keeping the edges of the lids from scarring over. Other factors that can disrupt the lipid layer such as side effects of medications like Accutane and putting eyeliner on the ‘water line’. Lid deformation/scarring often results from atrophy of the meibomian glands after decades of chronic clogging.
Treatment can significantly improve the issues related to lid health in most cases. However, once your oil glands atrophy due to prolonged clogging, they cannot be restored. Clearing obstructions, reducing inflammation to avoid future scarring, and utilizing thermal therapies in combination with gland expression prove effective in almost all cases of MGD.
Huge numbers of patients need Thermal Therapies for dry eye, only small percentage getting it
When you consider how prevalent this type of dry eye is in the general population, eye doctors need to have an effective way to treat it. In a study of optometrists and ophthalmologists who treat dry eye and related ocular surface disease from 2021, 87% of these physicians agreed that obstruction of meibomian glands is a vital component of MGD. In addition, 71% of these eye doctors said that obstruction removal (clearing out the glands) should be the first step in treatment of MGD. Yet only 5% of patients surveyed received thermal therapies.

This .gif shows how much clogged oil we can get out of meibomian glands. Expression and imaging by Dr. Mark Cannon in Seattle, Washington
This means that while the vast majority of providers recognize the importance of managing and treating MGD, very few are incorporating MGD treatments into their medical practice. Dr. Cannon has been coaching patients on how to do a warm compress followed by lid massage at home for many years. New technologies and studies have made it clear that expressing these oil glands professionally can make a big difference by allowing the lids to make and release healthy oils again. As a result, Cannon EyeCare is incorporating thermal expression into our in-office treatments.
New “Thermal Gland Expression” appointment type available at Cannon EyeCare
In-office treatments such as a deep cleaning of the lids with the NuLids device can help. So can heating the lids to the desired temperature, followed by manual expression of the glands. This combination of treatments can be more effective and speed the relief of symptoms when a hot compress and lid massage at home are not enough. This next-level of dry eye management is safe and effective, yet for many patients the procedure itself is uncomfortable. It might even make your eyes sore for a few days afterward. Doctors can prescribe a steroid eye drop for patients experiencing discomfort more than one day after thermal therapies. This helps to calm down the related inflammation. Most patients only need non-preserved artificial tears and maybe a high-quality omega-3 oral supplement.
Blinking counts for a lot
You may be wondering what the connection is with blinking and dry eye. We have about 50 of these specialized oil glands in our lids (the Meibomian glands). They should be releasing healthy oils into our tears with every blink. But this only happens when we do a proper blink. A good blink is when the lids come all the way together and then press upon each other with a bit of opposing force for about a second. This causes the edge of the lid to wrinkle or ‘crumple’, thus shortening the lid for a second.
This shortening or compaction of the lid is what actually pumps the oils out of your glands. So if you don’t blink well enough, these glands are not going to be releasing their oils into your tears. A lack of healthy oil in the tears causes the tears you do have to evaporate too quickly, thus causing dry eye.

Have you been suffering from Dry eye or MGD? Thermal therapies for dry eye and MGD could be the solution you’re looking for. In this article you can get all the information you need about Dry Eye and Meibomian Gland Dysfunction (MGD) and how you can treat them with Thermal Therapies for dry eye.
What Is MGD?
Meibomian Gland Dysfunction (MGD) is a condition characterized by the dysfunction or blockage of the meibomian glands, which are located in the eyelids. These glands produce the oily component of the tear film (meibum) that coats the ocular surface, helps lubricate the eyes and prevent tears from evaporating too quickly.
What Is Dry Eye?
Dry eye, also known as dry eye syndrome, dry eye disease, ocular surface disease or keratoconjunctivitis sicca, is a common condition that occurs when there is a lack of sufficient moisture or lubrication on the surface of the eyes. It can result from either decreased tear production or increased tear evaporation. Recent studies have shown that about half of Americans will experience dry eye as they age.
Is MGD The Same Thing As Dry Eye?
Meibomian Gland Dysfunction (MGD) and dry eye are often grouped together because they exhibit similar symptoms, including irritation, intermittent blur, itching, and/or burning. However, the underlying causes differ, and in fact there are 2 main types of dry eye: aqueous deficient (when there’s a lack of liquid tears production) and evaporative dry eye, which involves MGD.
Evaporative dry eye is what you’ve got if the tears you do have are poor quality. Having poor-quality tears means that your tears are unstable and evaporate too quickly. This is what our eye doctors are checking when they have you try not to blink at the bright blue light for a full 10 seconds. If the eye doctor observes a Tear Break-Up Time (TBUT) of less than 10 seconds, that is a sign of evaporative dry eye. Recent studies have shown that 86% of patients symptomatic for dryness have the evaporative type. So if your eyes are dry, the odds are good that you have underlying MGD. It is noteworthy that you can have both the aqueous and evaporative forms of dry eye.
Dr. Mark Cannon now has advanced imaging capability at our Pike Place office. He routinely captures infra-red images of the meibomian glands for our dry eye patients with our new advanced Firefly slit lamp microscope.

Evaporative & Aqueous Dry Eye
Recognizing the distinction between evaporative and aqueous dry eye is crucial when selecting an appropriate treatment.
In terms of tear composition, the tear film consists of three layers. The oily layer, produced by the meibomian glands, prevents rapid evaporation of tears and maintains a smooth surface. The watery layer, generated by the lacrimal glands, constitutes the actual tears. Lastly, the mucus layer, created by the conjunctiva, aids in spreading the tears evenly.
In cases of MGD, the meibomian glands fail to secrete sufficient healthy oils due to clogging of the exit pore or the oils being too thick – like butter or crisco. If the miebomian glands are not releasing oils frequently due to poor blinking or chronic clogging, the glands can atrophy – See image above. Often times the oily secretions will flow if forced, but are too thick and poor quality to move without intervention.
Consequently, tears evaporate too quickly (a fast TBUT), leading to dryness in the eyes. On the other hand, aqueous dry eye occurs when the lacrimal glands are unable to produce an adequate volume of tears. This may be caused by factors such as gland damage, medication usage, or medical conditions like Sjogrens Disease diabetes and lupus. Additionally, liquid tear production can be greatly effected by hydration levels and naturally slows down with age. The vast majority of Dr. Mark Cannon’s dry eye patients start out chronically dehydrated when they first seek him out for treatment.
Both MGD and aqueous dry eye can be treated, although our therapeutic approaches differ.
Recent investigations into dry eye disease have found that 86% of dry eye patients have Meibomian Gland Dysfunction (MGD). There are a number of things that cause MGD, such as aging, blepharitis, and lots of screen time. Another big factor is how thoroughly you blink; more on that later in this post.
Eye doctors have become increasingly aware of the importance of healthy, functional meibomian glands in recent years. The oils they release into the tears (creating the ‘lipid layer’) from the edge of your lid are a key component to healthy tears. If the glands are clogged or blocked, your tear quality will suffer as a result. This causes quick evaporation of the watery portion of your tears, with a resulting intermittent blur and discomfort or burning.
Your optometrist or ophthalmologist can determine how many glands are currently obstructed by pressing gently on your lids in a few different spots. Many offices (including Cannon EyeCare at Pike Place’s Market Optical) have specialized infra-red cameras that can image these meibomian glands. Often getting a baseline image is useful to track for future changes. This type of imaging is inexpensive and we can often bill the cost to insurance. We like to capture imaging of the meibomian glands annually to watch for change.
What To Consider When using Thermal Therapies for dry eye and MGD?
When addressing MGD, it’s important to recognize that two factors require attention: addressing obstruction and inflammation of the gland. The gland obstruction issue involves the physical blockage of the exit port for the gland. Obstructions can be removed by treating an overgrowth of bacteria on the lids known as blepharitis, eliminating an infestation of the lash follicles by Demodex mites, and keeping the edges of the lids from scarring over. Other factors that can disrupt the lipid layer such as side effects of medications like Accutane and putting eyeliner on the ‘water line’. Lid deformation/scarring often results from atrophy of the meibomian glands after decades of chronic clogging.
Treatment can significantly improve the issues related to lid health in most cases. However, once your oil glands atrophy due to prolonged clogging, they cannot be restored. Clearing obstructions, reducing inflammation to avoid future scarring, and utilizing thermal therapies in combination with gland expression prove effective in almost all cases of MGD.
Huge numbers of patients need Thermal Therapies for dry eye, only small percentage getting it
When you consider how prevalent this type of dry eye is in the general population, eye doctors need to have an effective way to treat it. In a study of optometrists and ophthalmologists who treat dry eye and related ocular surface disease from 2021, 87% of these physicians agreed that obstruction of meibomian glands is a vital component of MGD. In addition, 71% of these eye doctors said that obstruction removal (clearing out the glands) should be the first step in treatment of MGD. Yet only 5% of patients surveyed received thermal therapies.

This .gif shows how much clogged oil we can get out of meibomian glands. Expression and imaging by Dr. Mark Cannon in Seattle, Washington
This means that while the vast majority of providers recognize the importance of managing and treating MGD, very few are incorporating MGD treatments into their medical practice. Dr. Cannon has been coaching patients on how to do a warm compress followed by lid massage at home for many years. New technologies and studies have made it clear that expressing these oil glands professionally can make a big difference by allowing the lids to make and release healthy oils again. As a result, Cannon EyeCare is incorporating thermal expression into our in-office treatments.
New “Thermal Gland Expression” appointment type available at Cannon EyeCare
In-office treatments such as a deep cleaning of the lids with the NuLids device can help. So can heating the lids to the desired temperature, followed by manual expression of the glands. This combination of treatments can be more effective and speed the relief of symptoms when a hot compress and lid massage at home are not enough. This next-level of dry eye management is safe and effective, yet for many patients the procedure itself is uncomfortable. It might even make your eyes sore for a few days afterward. Doctors can prescribe a steroid eye drop for patients experiencing discomfort more than one day after thermal therapies. This helps to calm down the related inflammation. Most patients only need non-preserved artificial tears and maybe a high-quality omega-3 oral supplement.
Blinking counts for a lot
You may be wondering what the connection is with blinking and dry eye. We have about 50 of these specialized oil glands in our lids (the Meibomian glands). They should be releasing healthy oils into our tears with every blink. But this only happens when we do a proper blink. A good blink is when the lids come all the way together and then press upon each other with a bit of opposing force for about a second. This causes the edge of the lid to wrinkle or ‘crumple’, thus shortening the lid for a second.
This shortening or compaction of the lid is what actually pumps the oils out of your glands. So if you don’t blink well enough, these glands are not going to be releasing their oils into your tears. A lack of healthy oil in the tears causes the tears you do have to evaporate too quickly, thus causing dry eye.
Pike Place Office
1906 Pike Pl Unit 8-b,
Seattle, WA 98101
University Village Office
2602 NE University Village St,
Seattle, WA 98105
Pike Place Office Hours
Monday
Closed
Tuesday
10:00 am - 5:00 pm
Wednesday
Closed
Thursday
10:00 am - 5:00 pm
Friday
10:00 am - 5:00 pm
Saturday
10:00 am - 5:00 pm
Sunday
Closed
University Village Office Hours
Monday
10:00 am - 6:00 pm
Tuesday
10:00 am - 6:00 pm
Wednesday
10:00 am - 6:00 pm
Thursday
10:00 am - 6:00 pm
Friday
10:00 am - 6:00 pm
Saturday
10:00 am - 6:00 pm
Sunday
Closed
